Minority and Indigenous Trends 2021: Lessons of the Covid-19 pandemic
It was clear, even in the early days of the pandemic, that minorities, indigenous peoples and other marginalized communities were at greater risk of infection and death from Covid-19. This was for a variety of reasons, ranging from limited access to health care and a higher prevalence of pre-existing illnesses to poverty and the concentration of many members in jobs and livelihoods that were hazardous or insecure.
Indeed, across the world, many frontline occupations such as delivery services, public transport and medical work are undertaken by members of these communities, working continuously throughout the first lockdowns when the rest of the population were being urged to stay at home for their own safety.
Subsequently, however, it has become apparent that the impacts of the crisis have extended far beyond the immediate health outcomes, with everything from employment and education to housing and mental well-being disrupted. In these areas, too, minorities and indigenous peoples have frequently borne a disproportionate burden, exacerbated in many countries by poorly implemented or discriminatory government policies. While the shared crisis of Covid-19 could have created momentum for solidarity and ceasefires, in reality persecution and conflict often appear to have escalated in the wake of the virus.
More fundamentally, however, much of the inequity and discrimination brought to the surface by the pandemic was present long before the outbreak – and is likely to remain in place without transformative societal change. As countries navigate the uncertain path towards recovery, it is vital that there is more than simply a return to normality. This painful global emergency also offers an opportunity to achieve lasting change to the systemic racism and injustice that minority and indigenous communities have contended with for generations. Without meaningful action to address these underlying issues, however, the world will continue to be exposed to the threat of further health crises in the years to come. With that in mind, this report outlines 10 key lessons for governments, societies and communities to follow for a fairer and more sustainable post-pandemic future.
Summary and thematic chapters
- 01

Executive Summary
It was clear, even in the early days of the pandemic, that minorities, indigenous peoples and other marginalized communities were at greater risk of infection and death from Covid-19. This was for a variety of reasons, ranging from limited…
0 min read
- 02
Foreword
by Tlaleng Mofokeng, UN Special Rapporteur on the right of everyone to the enjoyment of the highest attainable standard of physical and mental health As the demands of the pandemic have evolved, from the initial scramble for masks and…
1 min read
- 03

Preface
By Joshua Castellino and Claire Thomas This report primarily focuses on minority and indigenous communities and their experiences during Covid-19. But we also turn our gaze inward briefly. In seeking to come to terms with the loss and the…
1 min read
- 04

Human rights and Covid-19: Repression and resistance in the midst of a pandemic
By Nicole Girard Covid-19 has exposed the stark inequalities existing in our societies. Minorities, indigenous peoples and migrant communities have been hit disproportionately by the spread of Covid-19, fuelled by poorer pre-existing…
1 min read
- 05

Livelihoods and employment: The impact of Covid-19 on the economic situation of minority and indigenous workers
By Rasha Al Saba and Samrawit Gougsa Amid a global recession triggered by the Covid-19 pandemic, minorities and indigenous peoples have been hit especially hard in the world of work. Not only have members of these communities lost their…
1 min read
- 06

Recognizing the right to health for minorities and indigenous peoples: Transforming the global inequalities of the pandemic into health justice
By Sridhar Venkatapuram The announcement by the World Health Organization (WHO) in January 2020 of a new and harmful infectious disease rightly raised the alarm among minorities and indigenous peoples around the world. Their concern,…
1 min read
-
It was clear, even in the early days of the pandemic, that minorities, indigenous peoples and other marginalized communities were at greater risk of infection and death from Covid-19. This was for a variety of reasons, ranging from limited access to health care and a higher prevalence of pre-existing illnesses to poverty and the concentration of many members in jobs and livelihoods that were hazardous or insecure.
Indeed, across the world, many frontline occupations such as delivery services, public transport and medical work are undertaken by members of these communities, working continuously throughout the first lockdowns when the rest of the population were being urged to stay at home for their own safety.
Subsequently, however, it has become apparent that the impacts of the crisis have extended far beyond the immediate health outcomes, with everything from employment and education to housing and mental well-being disrupted. In these areas, too, minorities and indigenous peoples have frequently borne a disproportionate burden, exacerbated in many countries by poorly implemented or discriminatory government policies. While the shared crisis of Covid-19 could have created momentum for solidarity and ceasefires, in reality persecution and conflict often appear to have escalated in the wake of the virus.
More fundamentally, however, much of the inequity and discrimination brought to the surface by the pandemic was present long before the outbreak – and is likely to remain in place without transformative societal change. As countries navigate the uncertain path towards recovery, it is vital that there is more than simply a return to normality. This painful global emergency also offers an opportunity to achieve lasting change to the systemic racism and injustice that minority and indigenous communities have contended with for generations. Without meaningful action to address these underlying issues, however, the world will continue to be exposed to the threat of further health crises in the years to come. With that in mind, this report outlines 10 key lessons for governments, societies and communities to follow for a fairer and more sustainable post-pandemic future.
Photo: A portrait of a man from the Khomani San of Kalahari community in South Africa. The reduction in tourism due to Covid-19 has impacted the community’s livelihoods. Credit: Tim Wege / Alamy.
-
by Tlaleng Mofokeng, UN Special Rapporteur on the right of everyone to the enjoyment of the highest attainable standard of physical and mental health
As the demands of the pandemic have evolved, from the initial scramble for masks and ventilators to the ongoing struggle to purchase vaccines — one that, predictably, the most affluent states have dominated despite the urgent need in many developing countries — there has been a great deal of discussion on how to ensure an equitable recovery. Quite rightly, much of this has focused on the wide gaps between richer and poorer nations. Yet it is just as important to ensure that similar disparities do not emerge within countries between more and less privileged groups.
From early on in the pandemic, it was clear that Black people, minorities, indigenous peoples and other racially and religiously persecuted groups were significantly more exposed to the threat of Covid-19 and greatly impacted by it. For them, however, the health crisis did not begin with the virus. Within the Global South, and deeply rooted in historical oppression, coloniality, systemic racism and structural discrimination, countries have less favourable health systems and face disparities and inequities to access the determinants of health. It is in this context that those populations in particular are affected by higher rates of infant mortality to lower life expectancy, from greater exposure to communicable disease like tuberculosis to a heavier burden of mental illness. Every stage of their lives has been characterized by disproportionately poorer health outcomes. The situation is especially acute for women, people with disabilities and LGBTQ+ and gender diverse persons, who often experience intersectional discrimination on account of their identity.
These disparities are not going away on their own. We are far away from a scenario of an equitable, global vaccine rollout that successfully reaches the many communities usually excluded from underlying determinants of health such as clean water and sanitation, let alone medical care. However, without this, of course, there is no guaranteed end in sight to the pandemic. Looking beyond our immediate predicament, there are broader lessons to be learned. Otherwise, for populations in the Global South, Black people, minorities, indigenous peoples and other discriminated groups, the crisis will simply continue in other forms – exposing them, as before, to disproportionate levels of death, disease and mental illness.
We now know that many factors can contribute to better protection from Covid-19, from effective hygiene and social distancing to safer working conditions. Though often described as ‘behaviours’, these are grounded in rights and needs – adequate housing, healthy occupational and environmental conditions, labour protections, equitable health systems – that are simply unattainable for many. Unless a rights-based approach is employed for communities forced to the margins, living in crowded apartments in low-income neighbourhoods or informal settlements without sanitation, these issues will remain long after the pandemic has ended.
The crisis of Covid-19 may be unprecedented, but the inequalities it has compounded have been with us for generations. The scale of the challenge we now face and the universal threat it poses demand much more than charity: to emerge from this catastrophe stronger, we need transformative change. This means, first and foremost, to address coloniality, an end to discrimination, inequality and other underlying conditions that have long undermined the health and security of minorities, indigenous peoples and other neglected groups. We need to fully embrace all human rights.
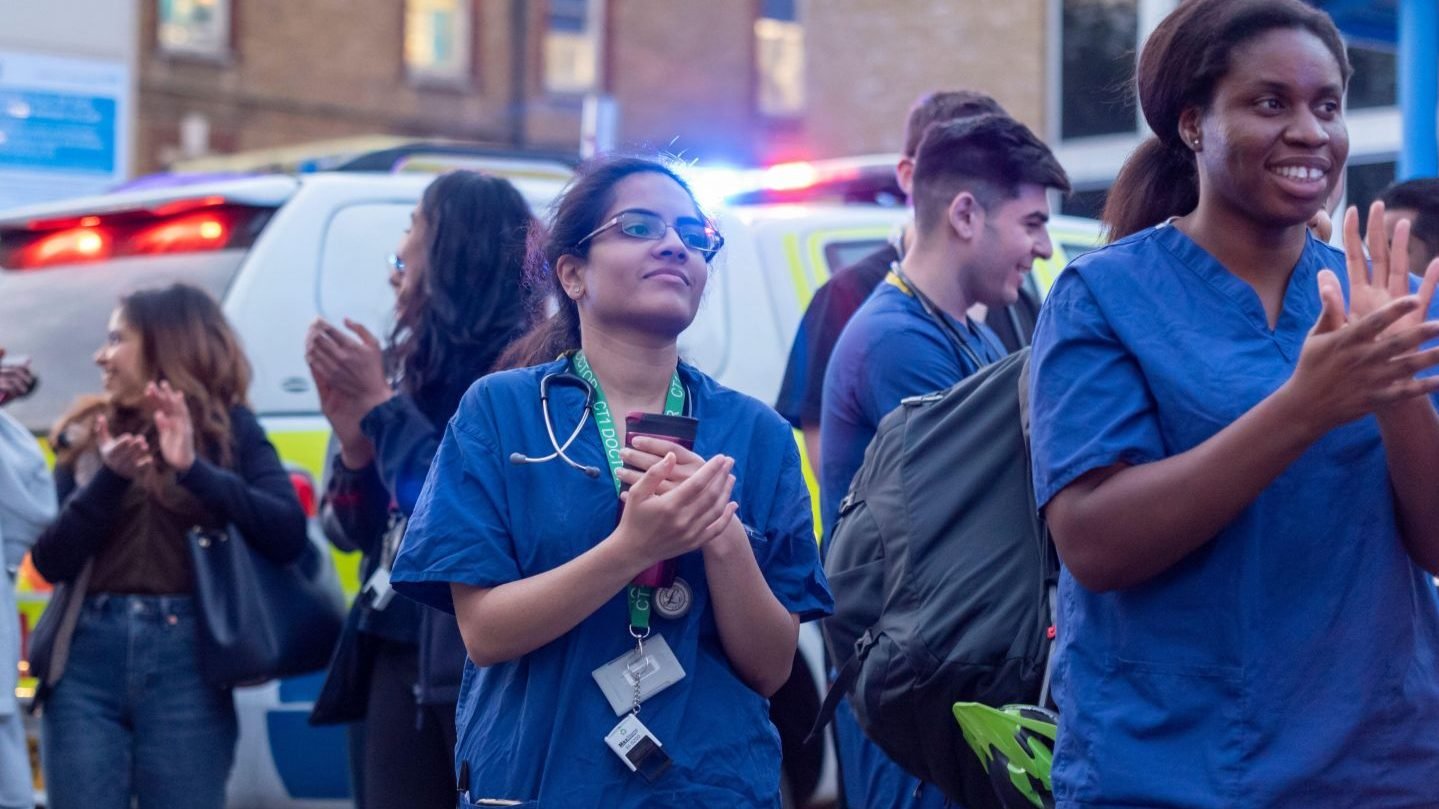
Photo: Ethnic minority health works gather with police and fire crews outside a hospital in London, UK, to ‘Clap for Carers’ as a sign of gratitude for the services of essential workers during the Covid-19 pandemic. Credit: Avpics / Alamy Stock Photo.
-
By Joshua Castellino and Claire Thomas
This report primarily focuses on minority and indigenous communities and their experiences during Covid-19. But we also turn our gaze inward briefly. In seeking to come to terms with the loss and the trauma inflicted by the pandemic, it is incumbent on us all to extract the painful lessons emerging from this experience to be better prepared for similar crises in future.
Our work at Minority Rights Group (MRG) interacts with many systems: international human rights mechanisms, development and aid provision, national advocacy and law making, judicial processes, service delivery and civil society solidarity. All of these were affected in some way by Covid-19, forcing us to rethink ways of working which, it turned out, were often dictated by habit and custom rather than necessitated by external realities.
One lesson we take away from this time is how to overcome our own resistance to change. Some ways of doing things may have changed permanently; others may revert back eventually (with or without good reason). Covid-19 highlighted how poorly designed systems were rendered ineffective in responding to a swift global challenge of this kind. In particular, it demonstrated how easily local, national and international solidarity broke down in the face of adversity. When faced with crisis, it seems, we mostly put our own needs first. Those with greater social, political or economic capital ‘won’ against those with lower status, who were less well connected or less well off. Combating these recurring patterns lies at the heart of the minority and indigenous rights and anti-discrimination mission that MRG exists for.
Prior to the pandemic, international human rights mechanisms had strongly resisted virtual participation in forums and debates. After initial postponements and cancellations, these objections were swept away and virtual participation is now routine. This has made involvement more egalitarian and cost effective but has also heightened the digital divide. Internet connectivity and equipment is not yet in place for all — with minority and indigenous communities disproportionately affected. Virtual attendance also fails to replicate the access to decision makers that ‘corridor’ lobbying normally provides, by speaking to decision makers face-to-face on the margins of physical meetings. It remains to be seen how this will settle post-pandemic. Retaining the benefits of virtual participation alongside some of the benefits of physical attendance may require designing virtual opportunities that simulate corridor lobbying online.
As an organization primarily funded to deliver restricted projects, we faced the challenge of needing to renegotiate a large number of contracts to pivot work into new directions as the original interventions were no longer possible, relevant or appropriate. This generated significant workload burdens and also led to delays in rolling out our responses. A more appropriate ‘disaster preparedness’ contract provision would have allowed donors to remove restrictions from a small proportion of restricted funding, limiting activities to the charitable objectives of the recipient organization or to project objectives without need for lengthy renegotiations. Such a mechanism could be triggered at the discretion of the donor during a global or national emergency, providing a swift, efficient and effective response by those who already have partnerships in place and are actively working to respond within their means to a crisis as it unfolds.
As the pandemic has highlighted, MRG’s work needs to continue whatever the conditions we face since our communities of concern will inevitably be pushed behind. It is therefore imperative for us to find innovative and effective ways to maintain the struggle, supporting marginalized communities and influencing institutions and the wider public until the systemic discrimination highlighted in this volume is a thing of the past. We hope the contents will provide you with insights, information, inspiration and motivation to join and accompany us on what is still a long and much needed journey towards equality, inclusion and participation for all.
Photo: Migrant workers carry their belongings as they walk along a road to return to their villages, during a 21-day nationwide lockdown to limit the spreading of Covid-19, in New Delhi, India, March 26, 2020. Credit: REUTERS/Danish Siddiqui.
-
By Nicole Girard
Covid-19 has exposed the stark inequalities existing in our societies. Minorities, indigenous peoples and migrant communities have been hit disproportionately by the spread of Covid-19, fuelled by poorer pre-existing health indicators, economic disenfranchisement and discrimination. But in many cases, it has been the government response to the pandemic that has exacerbated existing discrimination, leading to increased insecurity and direct threats to minority and indigenous rights.
While temporary and balanced restrictions are necessary to address virus transmission, these public health measures must be carried out in proportionate, rights-respecting, non-discriminatory ways. What many communities have witnessed since the onset of the pandemic, however, has been repression – heavy-handed measures that were often not conducive to protecting public health, or even counterproductive to these aims, many either targeting minorities and indigenous peoples directly or impacting on them disproportionately.
These restrictive new measures have been undertaken often by emergency order or decree, with limited oversight, infringing on a broad range of human rights and often implemented in a discriminatory manner. Freedom of movement restrictions and associated fines have frequently targeted ethnic or religious minorities and other marginalized communities in particular. Blanket bans on freedom of assembly were implemented in scores of states worldwide, including those intended to stop minority protests, as in Turkey.
Contact tracing apps are threatening privacy rights, particularly for marginalized communities that have few options but to use them, such as migrant workers in Singapore, whose return to work entailed the non-optional use of sketchy contact tracing apps. Sweeping changes have been made in many countries without clear scientific justification or an exit strategy, and without engaging vulnerable communities or mitigating potential negative impacts.
This chapter will look at how a biosecurity response to the pandemic has exacerbated the impact of Covid-19 on minority, indigenous and migrant communities. This approach further entrenches inequality by prioritizing socio-economic and political interests, viewing people only as potential carriers, and enforcing top-down, authoritarian and military interventions to ensure public health compliance. There is little consideration of the complicated impact these measures have on people facing intersectional discrimination and, in some cases, the pandemic has been used as a pretext to further undermine minority and indigenous rights protections.
At the same time, biosecurity approaches have been a catalyst for community organizing unseen on such a broad scale in decades. Minority and indigenous communities are calling for a rights-based approach to the pandemic that puts systemic discrimination front and centre to address the underlying reasons for its spread, stepping in to assist their communities where the government has failed to do so, and resisting oppressive measures implemented under the cover of Covid-19.
Quarantining communities in Bulgaria: Discriminatory measures against Roma neighbourhoods
Racist and discriminatory approaches to public health during the initial spread of Covid-19 resulted in segregation and restrictions on movement for entire neighbourhoods and settlements, as was the case for Roma in Bulgaria and Slovakia, and refugee camps in Greece, where lockdowns targeted residents while the rest of the country had returned to normal. Non-governmental organization (NGO) Médecins Sans Frontières called the extended lockdown for refugee camps ‘absolutely unjustified from a public health point of view – it is discriminatory towards people that don’t represent a risk and contributes to their stigmatization, while putting them further at risk’ by keeping them in overcrowded and unhygienic conditions.
In Bulgaria, the extreme right Bulgaria National Movement (VMRO) exploited the crisis in what some Roma rights activists described as the ‘ethnicization of the pandemic’. In the early days of the emergency, VMRO chairperson and Bulgarian Member of the European Parliament (MEP) Angel Dzhambazki called for the closure of Roma neighbourhoods, describing them as ‘real nests of infection’. Shortly afterwards, the Kvartal Karmen settlement in the town of Kazanlak was blockaded, exits to the neighbourhood were sealed and the one remaining access point was continuously guarded by law enforcement. Similar checkpoints were installed around Roma settlements across various municipalities, leading to an overwhelming presence of soldiers, police and drones – constituting a far more visible presence than medical workers and supplies. In some instances, authorities did not ensure that blockaded communities had access to food, water or medicine: in Tsarevo, for example, 500 Roma residents were left without water for 10 days. Similar blockades were not instituted in non-Roma neighbourhoods, and churches remained open.
As blockades and checkpoints continued, Roma citizens began protesting in Sofia in mid-April 2020. Working largely in informal industries, many could not provide the documents necessary to allow them to pass through checkpoints. Rumours that Roma in certain neighbourhoods were infected prompted employers to fire workers. Roma activists submitted a citizens’ petition to the two other Bulgarian MEPs, calling for them to refute the words of Dzhambazki, but were met by silence. After sustained pressure, the restrictions were lifted at the end of April. Finally, in mid-May, two UN Special Rapporteurs on racism and minority issues released a joint statement calling the actions of the Bulgarian authorities ‘discriminatory’, ‘overly-securitized’, and ‘a violation of Roma’s right to equality and freedom of movement’ through ‘a government response to Covid-19 that singles out Roma’.
Stay-at-home orders in South Africa: Black women faced a surge in gender-based violence
As governments began to acknowledge the gravity of the emerging health crisis, lockdown policies were rolled out with varying degrees of severity worldwide. Some manner of lockdown was likely necessary at this stage to effectively contain the virus, but the disproportionate impact on vulnerable communities was often not considered, nor the effectiveness of standardized preventive measures in certain contexts. For example, for remote indigenous communities that were prevented from gathering forest products, such as in Cambodia, it is questionable whether restricting these livelihood activities would have any impact on spread that was at the time concentrated in urban settings. Similarly, nomadic pastoralists were prevented from making their traditional movements between Mauritania, Senegal and Mali, resulting in lack of land to graze their animals; this led, in turn, to overgrazing and increased tensions with settled communities. Lockdowns are more challenging for already vulnerable groups, resulting in an accumulating ‘health debt’ that is compounded by loss of income, mental health problems, discontinuity of any support systems and inadequate or non-existent social protection mechanisms.
Gender-based violence in particular skyrocketed during lockdown, with nearly every country in the world reporting an increase in calls to domestic violence hotlines and women seeking help in shelters and from the police. In some countries, such as Zimbabwe, women’s shelters were not recognized as essential services; this meant that survivors struggled to reach them as they could not get the essential services permits necessary for travel to access help. In any case, service providers had to close on account of their being classified as non-essential. For minority and indigenous women and girls, this situation is compounded by the discrimination they face both on account of their gender and as members of marginalized communities. They are frequently more vulnerable to violence than majority communities, stemming from a myriad of factors including socio-economic struggles, lack of engagement by state support systems and intergenerational trauma. Many of the statistics on reported incidents of male violence against women during lockdown do not disaggregate for ethnicity or other factors, but anecdotal evidence suggests that existing patterns of violence against minority and indigenous women were magnified both during lockdowns and in their wake. For instance, a community group working with indigenous San in the Omaheke region of Namibia reported that domestic violence had increased as a result of stay-at-home policies. When San farm labourers were dismissed without pay in March 2020, the resulting tensions and frustrations led directly to an escalation in domestic violence.
South Africa, one of the most dangerous places in the world to be a woman, had one of the strictest lockdowns in the world. Patterns of violence in this country expose poor Black women to disproportionate levels of violence, including femicide. After a nine-week lockdown was eased, murders of women took a significant leap, with 21 mostly Black women killed in the first two weeks. While the Minister of Police stated that crimes overall had decreased during lockdown due to a ban on alcohol sales, with the prevailing idea being that the return to selling alcohol had fuelled the increase in femicides, women’s rights advocates were quick to point out that calls to women’s help centres surged by 54 per cent throughout lockdown, in all provinces. Shelters were overwhelmed. One victim during this time was Altecia Kortje, who reportedly sought a protection order against her husband but was told by police to wait until restrictions had lifted: a week later, she was murdered by him along with their daughter. President Cyril Ramaphosa mourned the surge in femicides in an address to the nation in June 2020 as a ‘second pandemic’, but neglected to mention the equally frequent killings of sexual minorities and gender non-conforming Black people.
After a nine-week lockdown was eased in South Africa, murders of women took a significant leap, with 21 mostly Black women killed in the first two weeks.
Lockdown in India: Migrants hit hardest by restrictions
The lack of consideration of how drastic measures carried out in the name of public health can prove devastating for already marginalized communities was perhaps most pronounced in India. No planning was put in place to mitigate the catastrophic results of the world’s largest lockdown for people with no access to social protection programmes. After a nationwide lockdown was suddenly announced on 24 March with no prior warning, millions of migrant workers, many of whom are from Dalit, Adivasi and other marginalized communities, had no other option but to march out of metropolises on foot after the rail system was shut down, with hundreds dying en route. The lockdown, imposed arbitrarily by the government of Prime Minister Narendra Modi with little or no prior consultation, showed scant regard for the security and well-being of millions of migrant workers. Far from protecting public health, it only served to corral people together in masses as they tried desperately to escape the cities.
Most were daily wage labourers, with no savings or social safety nets, and so forced to return to their rural homes. Dalits have reported facing stigmatization upon return, both as outcasts and suspected carriers of the virus. Government work schemes and ration programmes have been criticized for not reaching the most vulnerable, but only benefiting higher castes. The lockdown was economically devastating for minorities: according to the COLLECT (Community-Led Local Entitlements and Claims Tracker) data initiative, increased debt was recorded among all of India’s minorities and indigenous peoples including Dalits, Muslims, Adivasis, and Nomadic and Denotified Tribes. Loss of livelihoods resulting in an increase in debt can lead to intergenerational forced and bonded labour.
Strikingly, as the situation in India rapidly deteriorated from March 2021, with a sharp spike in infections and deaths, many urban migrant workers again uprooted themselves from cities across the country to return to their villages. Fear of the rapid spread of the virus and the government’s ongoing failure to contain the unfolding tragedy drove these departures, despite the absence this time of a nationally imposed lockdown. Their exodus was undoubtedly inspired, too, by the trauma of their treatment a year before: in the words of Arundhati Roy, writing for The Guardian, ‘They’ve left because they know that even though they make up the engine of the economy in this huge country, when a crisis comes, in the eyes of this administration, they simply don’t exist.’
Insecurity in Colombia: Targeted violence on the rise
Most of the states that instituted nationwide lockdowns did not have prior experience of doing so, certainly not in the name of public health. The ways in which lockdowns — instituted with such urgency — would play out in existing conflict dynamics was not properly taken into account in many circumstances, leaving marginalized communities in the crossfire. In Mexico, for example, the lockdown was used by narco-traffickers and paramilitaries to expand territorial control at the expense of indigenous peoples, especially in the southern states of Chiapas and Oaxaca. ‘There is no pandemic for the paramilitaries’, explained Rubén Moreno, an indigenous rights activist from Chiapas in an interview with Equal Times. ‘Paramilitaries continue their violent actions, and indigenous people have no access to justice. This is absolute discrimination — and why does it exist? Because we are indigenous.’
In Colombia, the government-ordered lockdown made indigenous human rights defenders more vulnerable to targeted killings and assassinations. While even before the pandemic Colombia was already regarded as the deadliest place in the world for environmental rights defenders, many of whom are indigenous or Afro-Colombian, the numbers of those killed increased in 2020. According to Colombian NGO Indepaz, 113 indigenous rights defenders were killed, around 25 per cent more than in 2019. During the nationwide lockdown, indigenous leaders lost or faced reduced protections from state security, including bodyguards or night patrols, at a time when — forcibly confined to their homes and unable to move in response to threats — it was easy to locate and kill them without witnesses in a public setting. Furthermore, with state forces focused on Covid-19, armed paramilitaries were able to reinforce and strengthen their activities. As summarized to Amnesty International by Danelly Estupiñán, a human rights defender with the Process of Black Communities (PCN) in Buenaventura, Colombia:
‘Our enemies are still killing us and it’s not difficult for them during the pandemic because we are all at home, complying with the mandatory quarantine which means nobody can move. But it seems that the people who want to silence us are moving around without any problem. We are seeing a pattern whereby illegal armed groups come to social leaders’ homes and kill them in front of their families. In some cases, they kill their relatives as well.’
The lockdown had further ramifications on recruitment by non-state armed groups of children, many of whom are indigenous or Afro-Colombian, with more than double the number of minors recruited in the period of January to April 2020 than the total reported for the whole of 2019. The increase in child recruitment is thought to have come from lockdown school closures, which removed the protective spaces that were buffering children from recruitment while parents struggled with the socio-economic pressures brought on by the pandemic response.
Faced with this alarming situation, compounded by the economic fallout of Covid-19, indigenous leaders organized a march to the capital of Bogotá to stage a minga – meaning shared work or joint effort in indigenous Quechua – to protest the continued killings of leaders and the slow implementation of the 2016 Peace Accord with FARC (Revolutionary Armed Forces of Colombia) rebels. The march began on 8 October 2020 in the south and south-west, convening first in Cali, then marching 600 kilometres to the capital, where thousands gathered on 19 October. Leaders demanded to be met by President Ivan Duque, who instead flew to Cartagena for a private event.
Despite the challenges of the pandemic and the threat of police violence against protests, indigenous activists have continued to mobilize during 2021, including holding large-scale demonstrations in the city of Cali in April. These actions are driven by a belief that without sustained action, the violence and abuses will simply continue. ‘Not even the pandemic will stop our movement’, said Hermes Pete, head of the Regional Indigenous Council of Cauca (CRIC), to Al Jazeera. ‘There is no other path but to keep fighting.’.
A community-led approach to containment: Māori checkpoints in New Zealand
Many governments, having delayed too long their response to the global spread of the virus, acted belatedly with knee-jerk, top-down responses that were not instituted through informed discussion with communities. It could be argued that governments did not have the experience or mechanisms in place to engage in rapid consultations to assess disproportionate impacts on vulnerable communities. But for indigenous peoples with established governance systems, there was a clear rationale for the response to be designed and initiated by indigenous communities, with the necessary funding in place to do so, in order to ensure effective and culturally appropriate action.
In New Zealand, Māori leaders realized that they must lead on the response to the virus in order to maximize the protection of their community. Māori swiftly organized themselves, with the support and operational presence of local police, to set up 40 community checkpoints across the country, strongly encouraging travellers not to continue into iwi (tribal) territory. Operating on a 24/7 basis, checkpoints offered safety advice for local essential workers who needed to pass.
According to community leader Tina Ngata, the checkpoints were a form of direct action that stemmed from their remembrance of how hard Māori were hit in previous epidemics, stemming back to the 1700s and waves of Western explorers. ‘It is easy to understand the unease Māori communities felt when Covid-19 arrived on our shores’, Ngata explained in the journal Overland. ‘When you further consider that not only has the state historically failed to protect our ancestors, but that the common Indigenous experience of colonization includes the use of disease as a genocidal weapon, then you can understand why we could not wait for anyone to come and save us.’
Their preventive action was met with criticism from right-leaning parties, questioning the legality of the checkpoints, claims which were refuted by the police. Community members, however, spoke warmly of the state-Māori collaboration, highlighting the positive engagement of police in the process — a welcome development in itself, given the long history of mistreatment and violence Māori have suffered from law enforcement.
According to Colombian NGO Indepaz, 113 indigenous rights defenders were killed in 2020, around 25 per cent more than in 2019.
Covid-19 and conflict: Escalating human rights abuses in Myanmar
Covid-19 added another layer of volatility to existing conflict situations, particularly for vulnerable communities fleeing violence, such as displaced persons, refugees and asylum-seekers. Some warring parties, however, appeared to treat it as an opportunity to tip the scales in their favour. On the very same day that the UN Secretary-General António Guterres called for a global ceasefire in order to focus on the fight against the spread of the virus, the Myanmar government made three announcements: Covid-19 was in Myanmar; the Arakanese Army (AA) was a terrorist organization; and websites spreading ‘fake news’ were to be shut down. All three announcements were to escalate the conflict in Rakhine state, complicate the response to the pandemic and highlight the Myanmar government’s disregard for the health and survival of its own people.
The AA is one of many of Myanmar’s armed ethnic organizations fighting for self-determination and political autonomy from the central government. While relatively newer than its counterparts, it has successfully countered the military, known as the Tatmadaw, in its home of Rakhine state at the expense of the local civilian populations who have faced reported atrocities from both sides. Declaring it a terrorist organization served the purpose of distinguishing it from other armed groups, criminalizing anyone who communicated with the AA, including journalists and humanitarian workers. Three journalists were arrested thereafter for interviewing the AA. This designation has prevented meaningful cooperation and coordination on a Covid-19 response. An internet shutdown in eight townships in Rakhine and Chin states, in part designed to create a stranglehold on AA communications since June 2019, combined with the shutdown of two key Rakhine state news organizations as designated ‘fake news’ outlets, meant that crucial information on Covid-19 was not reaching key populations. Conveniently, these two news organizations are those that are doing on-the-ground reporting of the conflict.
While the government heeded the call for a ceasefire on 9 May 2020 in relation to its numerous other conflicts, this did not apply to the AA. Conflict continued to rage in the state, with the numbers of those displaced doubling throughout 2020 to reach over 100,000. Covid-19 infections in Myanmar have been most numerous in Rakhine, with random testing in camps for displaced persons suggesting that community transmission is widespread – unsurprisingly, given the cramped and unsanitary conditions. The deadly effect of the conflict on the pandemic response was epitomized by the 20 April killing of a World Health Organization (WHO) driver who was delivering Covid-19 test results in a marked WHO van. Both the Tatmadaw and AA denied responsibility. In September, 70 people fled a quarantine centre in western Rakhine state after a night of nearby fighting. ‘We do want to stay at home but we can’t’, explained a villager sheltering at a monastery to The Irrawaddy newspaper. ‘Though we are afraid of coronavirus, we are also afraid that artillery shells might fall.’
Aid from the government in response to Covid-19 has been limited and poorly organized. At the very start of the pandemic, six Sittwe-based local civil society organizations established the Arakan Humanitarian Coordination Team (AHCT) to coordinate humanitarian assistance to those in Rakhine. They work both with the government and international donors to coordinate efforts, including for overlooked displaced populations who are not residing in established camps. They have also set up community quarantine centres and provided necessary supplies. Restrictions on movement have had serious consequences for aid and relief, with organizations required to secure official clearance to go to the camps to provide assistance, and with negative Covid-19 tests required just to drop off supplies. Even with permission, they are stopped at military checkpoints and, in October 2020, an authorized boat carrying supplies for the ICRC (International Committee of the Red Cross) was attacked by the Myanmar navy, killing the captain and damaging the vessel.
After elections in November saw a landslide win for the National League for Democracy (NLD), the military seized power on 1 February 2021 and used the Covid-19 crisis to justify, realize and solidify their rule. NLD chairperson and State Counsellor Aung San Suu Kyi was arrested and charged with ‘breaching Covid-19 restrictions’ under a recently junta-altered section of the Penal Code. Anti-Covid measures have been used to justify swift and brutal crackdowns on the population. The military actively suppressed the responses of armed ethnic organizations to Covid-19 before it seized power, and it continues to be the primary impediment to an effective response in the country, despite presenting the pandemic as a pretext for its illegal actions.
Business as usual: Land grabbing and deforestation in Indonesia
The Covid-19 pandemic has given governments the opportunity to rush through controversial laws, policies and practices under the guise of economic recovery. According to a Forest Peoples Programme report covering countries with the largest remaining tracts of tropical forests – Brazil, Colombia, the Democratic Republic of the Congo, Indonesia and Peru – social and environmental safeguards were rolled back extensively in 2020. States are prioritizing expansion of mining and logging, infrastructure development, agro-business and the energy sector in or near indigenous territories with little regard for existing rights protections, enacting new land use regulations and corporate stimulus packages at the expense of existing consultation mechanisms. Similar trends have been recorded in Honduras, India and the Philippines. Urban inhabitants returning to rural areas in response to lockdowns further increased pressure on forests. As a result, according to data from Global Land Analysis and Discovery (GLAD) – a worldwide warning system for the depletion of tree cover that uses satellite data – global deforestation rates surged in 2020, increasing by 77 per cent compared to the previous three-year average.
In Indonesia, the first 20 weeks of 2020 saw a 50 per cent increase in loss of forests compared to the same period in 2019, according to GLAD. Despite this alarming situation, the Indonesian government decided to push forward legislation that will further erode indigenous rights to land and their crucial role in forest preservation. The Workplace Creation Law, referred to as the Omnibus Law, was passed by parliament in October 2020 and enacted by President Joko Widodo overnight on 3 November. It is essentially a neoliberal deregulation package, promoted as a means to streamline economic rejuvenation, that makes more than a thousand amendments to 79 laws, dissolving existing indigenous, local community and labour rights by removing environmental and social impact assessments; deregulating mining; reducing penalties for environmental violations; and excluding indigenous peoples from consultation processes. Massive street protests across Indonesia accompanied the bill’s passage, uniting the labour, student, indigenous and environmental movements, and resulting in thousands of arrests. Some were simply detained for online posts opposing the bill.
A coalition of Indonesian indigenous organizations submitted an urgent complaint to the UN Committee on the Elimination of Racial Discrimination (CERD), noting that: ‘Rather than respecting indigenous peoples’ rights and the advice of human rights experts, the Indonesian government has instead used the Covid-19 pandemic to rush through approval of the Law, hold discussions over the Law without notifying the public or consulting with affected rights holders, and vote on the Law without the required quorum of members of Parliament physically present.’
In Indonesia, the first 20 weeks of 2020 saw a 50 per cent increase in loss of forests compared to the same period in 2019.
Consolidating power: Turkey’s crackdown on dissent
Covid-19 has also been used as an opportunity to deflect attention from the actions of unpopular governments and bolster low approval ratings. In what was referred to as the ‘coronavirus polling bump’, many governments significantly increased their popularity in the first weeks of the pandemic, a common phenomenon during times of crisis. According to the Metropol Research Company, Turkish President Recep Tayyip Erdoğan’s approval rating jumped from 41.9 per cent in February 2020 to 55.9 per cent in March, its highest point since the attempted coup in 2016. Riding high on this new-found approval, laws increasing government control over media, social media, academia and civil society were passed, as Erdoğan continued to consolidate power and weaken the opposition.
The pandemic emboldened Erdoğan’s attacks on the pro-Kurdish People’s Democratic Party (HDP), as he continued to remove and arrest democratically elected HDP mayors, replacing them with hand-picked appointed trustees. While his campaign to remove HDP mayors began immediately after the elections in March 2019, in the first three months of the pandemic, trustees were appointed in 14 municipalities, primarily in the Kurdish south-east, and by the end of 2020, 48 out of 65 HDP mayors had been replaced, with 19 in pre-trial detention. This occurred despite the considerable disruption this entailed for a concerted pandemic response in these areas: after Turkey recorded its first Covid-19 case on 11 March, HDP mayors had played an active role in organizing relief efforts in their communities.
The south-eastern municipality of Batman, for example, had postponed water bills as a pandemic relief measure and was one of the first to have a trustee appointed. As 90 per cent of residents in Batman speak Kurdish, the HDP mayor had ensured that Kurdish-language versions were included in municipal settings, such as traffic signs. However, the appointed trustee immediately removed bilingual signage, leaving only Turkish. This lack of respect for minority language rights has also hampered an effective Covid-19 response. ‘Since the government has not provided services in our mother tongue’, a senior HDP representative told The National newspaper, ‘people cannot properly benefit from health services. All the posters and pamphlets on coronavirus precautions are prepared in Turkish and most people do not understand.’
As a response to lack of support from the central government, HDP initiated the ‘Sister Families campaign’ in March 2020 to encourage solidarity between families, pairing better-off households with those that were struggling economically to provide packages of basic necessities. Over 60,000 families were assisted by the programme. However, government-aligned media outlets described the campaign as ‘aiding a terrorist organization’. The government detained, and has filed lawsuits against, HDP representatives and volunteers who were implementing the campaign in many different cities.
In June 2020, two HDP deputies, Leyla Güven and Musa Farisoğulları, were stripped of their parliamentary seats and imprisoned on terrorism charges, accused of being members of banned militant Kurdish PKK (Kurdistan Workers’ Party) organization. In response, HDP organized a two-track ‘Democracy March’, which was planned to start from both the north-western province of Edirne and the south-eastern province of Hakkari and converge in the capital, Ankara. Soon after, protests were banned in 12 cities by their respective governorships, ostensibly to limit the spread of coronavirus. Most of these bans were only for a couple of days, which would mostly stop the protests, not the spread of coronavirus. Despite the bans, protests were held in 11 provinces and were met with police use of force and detentions of protesters. In December, Leyla Güven was sentenced to 22 years in prison. As the pandemic continues, the government has persisted in its campaign to silence the HDP, with a state prosecutor filing a formal request in March 2021 for the party to be outlawed in its entirety – a move condemned by its supporters as a calculated blow to democracy in the country.
Public health as a pretext for anti-migrant policies: Title 42 in the United States
The pandemic resulted in an unprecedented shutdown of borders worldwide, impacting in particular those fleeing violence and seeking protection. By 1 April 2020, over 91 per cent of the world lived in states restricting all international arrivals, and 39 per cent in states with total border shutdowns for non-citizens and non-residents. Border militarization intensified in numerous states, accompanied by nationalist rhetoric that wove xenophobic language together with ‘battling’ against the coronavirus. Hungarian Prime Minister Viktor Orbán blamed the spread of Covid-19 on illegal migrants and shut the country’s borders to asylum-seekers, while ignoring the significant occurrence of hospital-acquired infections spreading in under-funded, unprepared public hospitals. European Union border guard agency Frontex used the pandemic to justify its existence and consolidate its role, blurring migration prevention and public health protection: ‘If we cannot control the external borders, we cannot control the spread of pandemics in Europe. Frontex plays a key role in ensuring effective protection of the external borders of the European Union not only against cross-border crime but also against health threats.’
Minority and indigenous asylum-seekers in particular bore the brunt of worldwide border closure measures. In April 2020, the Malaysian air force denied entry to a boat carrying approximately 200 Rohingya refugees who had either fled from Myanmar or from camps in Bangladesh, citing concerns that they would bring the coronavirus into the country. Around the same time, the Bangladesh coast guard rescued boats with nearly 400 Rohingya on board: they had reportedly been turned away from Malaysia, with dozens dying as a result. Maritime expulsions were recorded in Malta and Italy as well.
Restrictive anti-immigrant and anti-refugee asylum procedures were a well-established cornerstone of US government policy throughout the administration of former US President Donald Trump. But the Covid-19 pandemic provided an opportunity to use public health law to expel up to 530,000 migrants and asylum-seekers and 16,000 unaccompanied children, an approach that would not have been possible under existing immigration law. On 20 March, the Centers for Disease Control and Prevention (CDC) issued a sweeping order to instantly reject all those arriving at the border without adequate entry documentation, systematically denying the right to asylum. The CDC was reportedly pressured by the Trump administration to issue the order – known as Title 42 – despite resistance from senior CDC officials. Public health and medical experts opposed the order in a joint statement, saying it was not based on science-driven public health measures, but rather was an example of ‘xenophobic, cruel, and unlawful policies implemented by the Trump administration under the pretext of public health’. The order was renewed multiple times throughout the year, and after a review initiated by the Biden administration, has continued into 2021, with the exception of its applicability to unaccompanied children. While Biden officials claim that those who need it can still seek protection, in the year of Title 42’s application fewer than 1 per cent of arrivals were able to do so.
While US Immigration and Customs Enforcement (ICE) does not collect disaggregated data on race or indigeneity, civil society workers report that a large proportion of those seeking asylum in the United States (US) are indigenous or Black. Given that indigenous asylum-seekers as well as Black Haitian Creole speakers face significant language barriers and more frequent forced family separation, these figures are particularly disturbing. The ICE detention centre system became ‘a massive Covid-19 hotspot’, according to the Haitian Bridge Alliance, an NGO working with Black migrants. Deportations and expulsions that were occurring in 2020 have been blamed for spreading the virus to South American countries, and particularly to remote and indigenous communities that many of the forcibly returned asylum-seekers came from. By April, over half of those returned on flights to Guatemala who were tested on arrival were found to be infected. Indigenous Guatemalan deportees reported stigmatization, and in some cases violence, from other community members upon their return.
In the US, the pandemic provided an opportunity to use public health law to expel up to 530,000 migrants and asylum-seekers and 16,000 unaccompanied children, an approach that would not have been possible under existing immigration law.
Technology and surveillance: Tracking Singapore’s migrant population
Some of the big winners in the Covid-19 crisis have been tech companies specializing in data collection, monitoring and surveillance. Many of the companies that have honed their expertise in migrant and refugee tracking, border control and law enforcement have been repackaging the technology for pandemic surveillance and policing initiatives. Contact tracing proximity apps, facial recognition, drones and thermal cameras have been proposed by companies and governments alike to control the spread of the virus, blurring the lines that might normally prevent the use of military tech on civilian populations. Border control systems and tools were used during the crackdown on Black Lives Matter protests following the murder of George Floyd in Minneapolis on 25 May 2020, with drone surveillance being fed into Homeland Security Department digital networks used by other federal agencies, violating the privacy rights of people exercising their right to protest. In the weeks following Floyd’s murder, however, Microsoft and Amazon announced that they would not sell facial recognition technology to the police in the US until federal legislation was in place, while IBM said it would stop selling the technology altogether due to its use in racial profiling.
The development of contact tracing apps, however, has surged forward in response to the pandemic, and they are often adopted through fast-track legislative or executive power procedures. While they can be designed to protect users — for example, by not storing personal data or collecting geolocation data — many Covid-19 contact tracing apps developed thus far are insecure and risk exposing users’ privacy and data. Also, given that many surveillance technologies tend to have been built on racially biased algorithms or are employed in ways that disproportionately impact minority, indigenous and other marginalized communities, it is particularly concerning that the rapid rollout of various Covid-19 surveillance technologies has not been accompanied by significant efforts to mitigate this potential impact.
Out of the over 40 countries that initiated digital proximity and contact tracing tools, Singapore was one of the first with the digital system TraceTogether, offered as an optional measure for the country’s citizens but imposed mandatorily on Singapore’s Covid-wracked migrant worker population. Hailing mostly from India, Bangladesh and China, hundreds of thousands of migrants work primarily in the construction and shipyard industries and reside in cramped dormitories. In these crowded and unsanitary conditions, infections quickly spread among migrant workers, who were then subjected to a brutal lock-and-seal programme. Following the end of their isolation, TraceTogether was required in order for them to return to work. The app was later supplemented by a Bluetooth-enabled ‘token’ to be worn on the worker’s wrist, also available to members of the wider population who might not have a smartphone, such as children and the elderly. While privacy and migrant worker advocates were concerned about TraceTogether data usage, assurances were fatally undermined when a government official admitted in January 2021 that the data could be accessed by police and in fact had already been used in a murder case. These troubling implications are being reflected in other countries across the world: once instituded, mandatory use of tracking technology will invariably be difficult to roll back and could be used to justify over-policing of minorities.
Biosecurity and public health: Policing the pandemic in Australia
A central issue connecting the different examples discussed in this chapter is the increasing cohesion between policing and public health, a securitized approach that tends to target or unfairly disadvantage minorities, indigenous peoples and migrant communities. In Canada, for example, ‘Public health has historically been an extension of policing for Black people.’ This is illustrated by the case of Africville, Nova Scotia, a predominantly Black community existing since the 1800s which was forcibly evicted in the 1960s on the pretext of a health risk due to the lack of a sewage system, instead of the authorities simply installing sanitation. Similar trends have been identified in more recent patterns of police stops, fines, detentions and arrests of Black people in relation to Covid-19. Indeed, reports from throughout the Global North show that minorities have been disproportionately targeted in Covid-related policing.
In anticipation of the pandemic’s likely impact on policing of minority and indigenous communities in Australia, a coalition of legal and human rights advocacy networks in collaboration with academics created an online portal to report instances of Covid-related stops by the police. This serves as a mechanism with which to monitor expanded police powers under lockdown and assess whether they are being applied without bias or prejudice. The data collected by the portal paints a sobering picture: Covid-related police stops and fines disproportionately targeted individuals from indigenous or Black communities. In an article analysing the portal’s data, the authors argued that the results demonstrated that the state is choosing criminalization over a public health paradigm:
‘We found Covid policing to provide opportunities for the intensification of longstanding and selective criminalisation processes, evident in the disproportionate focus on First Nations peoples in street policing and the high-visibility policing of racialised and socio-economically disadvantaged communities in public housing.’
Using a biosecurity approach to public health essentially pits communities against virus prevention measures: rather than building solidarity and informed action in bottom-up participatory approaches, communities are disempowered and treated as complicit in the spread. Bullying by law enforcement in the name of public health has been shown to weaken adherence to preventive measures and undermine the trust that is essential in promoting compliance.
Out of the over 40 countries that initiated digital proximity and contact tracing tools, Singapore was one of the first with the digital system TraceTogether, offered as an optional measure for citizens but imposed mandatorily on migrant workers.
Art and activism in the wake of Covid-19: Imagining the post-pandemic future
The year 2020 was one of seismic changes across societies worldwide, triggered by the upheaval brought about both by the virus itself and the response by many governments ostensibly intended to address it. But the onset of the pandemic also converged with the murder of George Floyd, creating an urgent momentum to push racism and injustice to the forefront of activism across the world.
According to Marshall Shorts, founding member of Deliver Black Dreams Maroon Arts Group based in Columbus, Ohio, 2020 witnessed the convergence of multiple pandemics: a moment when people were forced to face questions of racism and violence which Black artists have been reckoning with for a long time. Maroon Arts Group is ensuring that these conversations around racism and inequality, particularly in the wake of Covid-19, continue to take place after the health crisis has passed, so that countries do not simply fall back into pre-pandemic patterns of racial disparity.
As the lockdown eased, the Greater Columbus Arts Council employed artists to paint murals on the plywood that was used to board up businesses during the demonstrations against Floyd’s death, as a way to bear witness to the protests but also provide a public platform against racism. As a follow-up to the project, Marshall’s group was commissioned to make a more permanent 5,000 square foot mural that says, ‘Deliver Black Dreams, It’s for All of Us’. Marshall says the mural has been used as a testament to the protests and to keep the conversation around race ongoing. He explains:
‘It’s a call to action… It is on all of us to Deliver Black Dreams, but it is also to say, we have to have a radical imagination of what this society can look like, and then take action toward that… What does Delivering Black Dreams look like in health care, education, safety?’
Conclusion
As we move towards a post-pandemic future, we must collectively remember how the pandemic has thrived on society’s structural inequalities and address these weaknesses so they cannot be exploited again. As vaccine rollout begins throughout the world, these same considerations on inequality need to be prioritized if we are to be able to collectively rise above these continuing challenges. If the remedies to the pandemic do not address structural discrimination, we will find ourselves struggling to move into a post-pandemic future. After all, ‘We are only as free of risk as the most vulnerable in society.’
The responses that have already been initiated by governments, as outlined in this chapter, may serve only to further facilitate the spread of the virus, entrenching discrimination, infringing rights and making it more difficult for civil society to resist these changes. The community resistance and collective organization that has also occurred during the pandemic leaves some hope that the ‘radical imagination’ of societies, premised on equality, will be realized as the world emerges from the trauma of Covid-19. Ensuring equity and human rights for all is the best means possible to strengthen our resilience in the face of further pandemics and other future shocks.
Recommendations
- Ensure a human rights-based approach to containing Covid-19: Struggles for rights protections are bound to increase as societal structures bear continuing impacts from the pandemic. Governments need to structure their wider response around rights protections, ensuring that any initiatives do not negatively impact on fundamental rights, such as the right to protest and the right to privacy. Emergency measures must not be used to silence dissent.
- Place communities front and centre of public health campaigns: Deep engagement and informed dialogues with communities are the best ways to increase effectiveness and compliance. Local innovations and inclusion are necessary to build collective responsibility and power.
- Enhance support for at-risk human rights defenders: Minority and indigenous rights defenders must be facilitated in their work supporting communities and responding to crisis. This includes journalists and other media workers who are trying to protect independent, non-biased reporting.
- Collect and publish disaggregated data on health outcomes: It is vital to know how minorities and indigenous peoples are specifically affected by the pandemic, as this will guide efforts to appropriately target assistance and treatment to the most vulnerable communities. To control the spread of the virus, it is necessary to understand how transmission is itself facilitated by discrimination.
- Recognize and address the intersectional impacts of the pandemic: Those suffering from discrimination on multiple and intersecting points of identity, such as gender, sexuality, age, ability and class, will be even more exposed during times of crisis. Overlooking their experiences in the midst of a pandemic not only jeopardizes the security of those most at risk, it also poses a threat to the rest of society.
- Ensure assistance is inclusive and equitable: Any responses to the pandemic, whether social support or vaccine rollout programmes, must recognize and mitigate the disproportionate impacts on the rights of minority and indigenous peoples. Furthermore, solutions must be found through engagement with the communities themselves.
- Challenge hate speech and misinformation: Governments and human rights bodies should publicly acknowledge the risks of discrimination enabling the spread of Covid-19 and take proactive action to protect minorities and indigenous peoples from hate, including through public education, incident monitoring and reporting.
Photo: Colombian indigenous people protest Colombia’s President Ivan Duque’s policies during an indigenous meeting called ‘Minga’ in Bogota, Colombia. Credit: REUTERS/Luisa Gonzalez.
-
By Rasha Al Saba and Samrawit Gougsa
Amid a global recession triggered by the Covid-19 pandemic, minorities and indigenous peoples have been hit especially hard in the world of work. Not only have members of these communities lost their sources of income, they have also been left vulnerable to work in unsafe and exploitative conditions.
This chapter explores the disproportionate impact of the pandemic on the livelihoods and incomes of minorities and indigenous peoples as the crisis has unfolded. In particular, it examines the limitations of the policies put in place by different governments to protect workers and their rights, the continued pattern of exploitation and abuses that minority and indigenous communities face in the labour market, and the way these issues overlap with deeper patterns of discrimination that pre-date the pandemic itself.*
Loss of jobs, income and livelihoods
Besides the direct effects on public health, a major consequence of the pandemic has been unemployment, with the International Labour Organization (ILO) reporting that 8.8 per cent of global working hours were lost in 2020 alone, equivalent to 255 million full-time jobs, resulting in an estimated US$3.7 trillion in lost income. While many jobs in the formal sector were protected through government schemes, the informal sector – where the majority (61 per cent) of the world’s workforce are engaged and where minorities and indigenous peoples are overwhelmingly represented – has been much worse affected. The very nature of the informal economy means workers do not have secure employment contracts, access to labour protections or social protection through their employment, leaving them more vulnerable to exploitation and financial instability. Moreover, the gendered nature of this should be noted, as over 90 per cent of women in low-income countries are employed informally, leading to an even more profound impact on them.
Migrant workers on the margins of the global economy
Migrant workers across the world are often employed informally and have been severely affected by Covid-19. Not only have many lost their jobs, but some have even been physically abandoned by their employers to fend for themselves. In Lebanon, for example, where the economy was already in crisis even before the pandemic, scores of predominantly Ethiopian migrant domestic workers were fired and left on the street outside their country’s consulate in the capital city, Beirut. Most of the women had little or no money and relied heavily on the support of non-government organizations (NGOs) as they waited to be repatriated.
The Covid-19 pandemic also placed a spotlight on the vital contributions of migrant workers in the agricultural sector in maintaining food supplies locally and internationally. Countries that rely heavily on foreign workers in this sector saw significant labour shortages, not necessarily due to Covid-19 itself, but instead the measures put in place by governments to restrict the spread of the virus, particularly travel and containment rules. For example, in Canada, every year farmers rely on an estimated 60,000 foreign workers, mainly from Mexico, Guatemala and Jamaica, to harvest their crops. In the early months of the pandemic, however, Ontario was the epicentre of the country’s Covid-19 outbreak, where more than 1,000 migrant farm workers tested positive. As a result, many employers enforced strict rules, in particular on the foreign workers, whose visas are attached to the farmers they work for, resulting in a power imbalance where workers could easily be sent back to their home countries. Indeed, many were dismissed after accusations by employers of not following their imposed restrictions.
Migrant workers in India, most of whom are from Dalit and Adivasi backgrounds, also faced difficulties. Following lockdown, tens of millions of migrant workers lost their work in urban areas and were forced to return home, often to rural villages, without any clear means of survival. Yet the situation facing Dalits and Adivasis in South Asia expands beyond India. In Nepal, for example, a survey by the Samata Foundation of 1,500 Dalit respondents found that over 80 per cent reported financial distress due to Covid-19 and the restrictions introduced to contain its spread, with 45 per cent having lost their jobs in the wake of the pandemic. The fact that the large majority of Dalits are daily wage workers makes them especially vulnerable to the economic crisis brought on by the pandemic, leaving them struggling to make ends meet. The impact of unemployment and reduced incomes on migrant workers is also felt by family members in their home regions who rely on remittances – a particularly significant issue in South Asia, where a major share of global remittances are channelled by migrant workers elsewhere in Asia, the Middle East, Europe and North America.
The pandemic has also heavily affected global garment supply chains, where minorities and indigenous peoples are often employed, as demand for clothing and apparel dramatically reduced. Many retailers were quick to cancel or postpone production orders which, in many cases, had already been fulfilled ahead of delivery. For example, according to the Bangladeshi Garment Manufacturers and Exporters Association, by April 2020 more than 1 million Bangladeshi garment workers had been sent home without pay or lost their jobs after Western clothing brands such as Primark and Matalan cancelled or suspended £2.4 billion of existing orders in the wake of the Covid-19 pandemic.
In many cases, the companies refused to pay for clothing that manufacturers had already produced, resulting in the closure of thousands of factories and millions of garment factory workers being left jobless, often without wages owed or severance pay. This exemplifies a clear power imbalance in the fashion and garment industry, whereby the upfront investment of labour is placed on workers in poorer economies who also take on the greatest burden of financial loss and risk. Moreover, such incidents are having a significant impact on the nutritional status of garment workers, as noted by a November 2020 global survey by the Worker Rights Consortium of garment workers in nine countries: 80 per cent of respondents with children reported that they were having to go hungry to feed their children.
In Nepal, a survey by the Samata Foundation of 1,500 Dalit respondents found that over 80 per cent were financially distressed due to Covid-19.
Indigenous livelihoods threatened as tourism slides
Like migrant workers, indigenous peoples are also disproportionately represented in the informal economy. As they often work in sectors heavily hit by the pandemic, particularly as a result of government measures to prevent the spread of the virus, they have experienced a severe impact on their livelihoods and traditional economies. One area that has been especially hard hit is the tourism sector as a result of lockdowns and travel restrictions. While at its worst the sector has been associated with exploitation and environmental degradation, it can also be a vital source of income and employment for many indigenous communities.
For example, due to the intimate knowledge of the land on which they have lived for centuries, the Khomani San of the Kalahari in South Africa offer hunting packages on their land around the Kgalagadi Transfrontier Park on a commercial basis, to make a living. However, once lockdowns were enforced and tourism ceased, demand for their services drastically diminished, in turn reducing their income and leaving the community facing starvation. Moreover, as is often the case with hunter-gatherer communities who have been dispossessed of their ancestral lands, some were charged with poaching when they entered the park to hunt for food for survival during lockdown.
Similarly, in Colombia and Venezuela, women from the Wayuu community of Alta Guajira depended heavily on tourism for their income. According to a report by the Continental Network of Indigenous Women of the Americas (CNIWA) published in May 2020, the shrinking tourism industry led to approximately 50 children facing a critical state of malnutrition due to lack of food and water. This example highlights the severe impact that income losses for women can have on indigenous communities more widely.
Yet in some cases indigenous businesses have proved to be more resilient to the economic shock posed by the disruption in tourism. In the United States (US), for example, a survey conducted by the Native Hawaiian Chambers of Commerce and the Office of Hawaiian Affairs found that only 25 per cent of Native Hawaiian businesses reported their business to be over 50 per cent dependent on the tourism sector. In comparison, an estimated 47 per cent of non-Hawaiian businesses reported their revenue to be over 50 per cent dependent on the industry. The findings suggest that although Native Hawaiian businesses were also affected by the Covid-19 pandemic, they will play a crucial role in the economic recovery of the island.
Though tourism is an important source of income for minority and indigenous communities, the disruptions to the sector caused by Covid-19 highlight the precarity of depending on this form of income generation. The Pacific Islands, for example, successfully managed to keep the number of Covid-19 infections low during the first year of the pandemic but have been unable to escape economic hardship due to the decrease in tourism. Unlike their neighbours, Australia and New Zealand, the smaller Pacific Island countries often rely on aid and remittances and are not in a position to roll out robust stimulus packages. One key lesson of the Covid-19 pandemic is to consider how to remedy this dependence on tourism for minority and indigenous communities across the world, so that their income is more resilient to such shocks.
Exploitation and forced labour
Exploitation and forced labour – defined by the ILO Forced Labour Convention (1930) (No. 29) as ‘all work or service which is exacted from any person under the threat of a penalty and for which the person has not offered himself or herself voluntarily’ – thrive on desperation and inequality, leaving minorities and indigenous peoples especially susceptible. While forced labour existed long before the pandemic, the rise in global unemployment since the outbreak of the Covid-19 pandemic has created an enabling environment for further abuses.
The use of forced Uyghur labour in PPE supply chains
Some sectors have seen a boom of business and supply that has matched an increasing trend of exploitation of workers belonging to minorities and indigenous communities. A clear example of this is the immense global demand for personal protective equipment (PPE), such as N95 face masks and medical gloves, with values increasing more than tenfold by early April 2020, according to the Society for Healthcare Organization Procurement Professionals. As various governments and businesses sought to produce PPE to match demand, reports began to emerge of abusive working conditions and human rights violations of minorities and indigenous peoples involved in the production of these goods. In China, for example, a New York Times investigation revealed that several companies were implicated in the exploitation of Uyghurs, a persecuted and largely Muslim ethnic minority, to produce medical masks in conditions of forced labour. Though the forced labour was being used by companies, the companies have been operating through a government-sponsored programme that many claim forces people to work against their will.
Slavery-like conditions in the Gulf
The Gulf states host the majority of an estimated 23 million migrant workers living in the Arab states. Though they are some of the richest countries in the world, with economies highly dependent on foreign labour, systematic abuse and exploitation of migrant workers has been well documented. Most notoriously, many migrant workers are subject to the ‘kafala’ system, which gives employers immense power and control over the lives of those on their payroll. Workers typically require the permission of their employers to change jobs and are often reliant on them for food, accommodation and legal documentation. Violations of migrant workers’ rights in the region include a lack of adequate health care; inhumane living conditions, including lack of adequate food and housing; and visa deprivation and non-payment of wages – situations that are indications of modern slavery.
The pandemic has caused a sharp increase in the abuse and exploitation of migrant workers in the Gulf, with the Business and Human Rights Resource Centre documenting a 275 per cent increase in reported labour abuses against migrant workers in Gulf countries between April and August 2020 alone. In 95 per cent of incidents, the victims cited Covid-19 as a ‘key or worsening factor’, while the most frequently cited abuse (81 per cent of all cases) was non-payment of wages. For those affected, challenging employers to recover unpaid wages has been especially difficult due to the extensive repatriation programmes carried out, often forcibly, on foreign workers.
In Saudi Arabia, a report by Equidem revealed that thousands of low-wage migrant workers employed by subcontractors for Saudi Aramco, the oil and gas conglomerate, were left unpaid for as long as six months during the Covid-19 pandemic. In the United Arab Emirates (UAE) too, thousands of construction workers employed on the Dubai Expo mega-project were dismissed without warning. Many of these workers, still owed unpaid wages, were returned to their home countries or forced to stay in poorly maintained accommodation.
Crowded together in unsanitary conditions and with limited access to health care, Covid-19 spread quickly among the Gulf’s migrant populations, triggering a wave of deportations and detentions, often in inhumane conditions. In Saudi Arabia, for example, Human Rights Watch reported in December 2020 that conditions in a deportation centre in Riyadh holding hundreds of mostly Ethiopian migrant workers were ‘so degrading that they amount to ill-treatment’. Detainees described unhygienic and overcrowded living conditions that made any kind of social distancing to prevent the spread of Covid-19 impossible; beatings were common, with at least three reports of deaths in detention.
In Qatar, meanwhile, some 2 million migrant workers make up about 95 per cent of the total labour force, sustained by the vast construction boom over the last decade ahead of the 2022 Fifa World Cup. Long before the pandemic, long working hours and limited labour protections were exacting a heavy toll on migrant workers: analysis published by The Guardian in February 2021 revealed that more than 6,500 migrants had died in the country since 2010, with little evidence of substantive investigations into the cause of many deaths. After hundreds of construction workers tested positive for Covid-19 at the start of the pandemic, Qatari police sealed off the country’s largest labour camp, leaving thousands of workers trapped in unsanitary and overcrowded living conditions that contributed to the high levels of infection among migrants.
The predicament of foreign workers in the country was made worse by the Qatari government’s decision, early on in the pandemic, to prioritize the interests of businesses over the well-being of workers: a government directive effectively suspended even the limited protections in place by permitting companies that had halted their activities as a result of restrictions to put employees on unpaid leave or terminate their contracts.
Forced marriage on the rise as economic pressures bite
The start of the pandemic has also been matched by a sharp increase in cases of forced marriage across the world. For ethnic minorities in Hong Kong, particularly South Asians, the disruption of schools and education, coupled with sudden job loss, led more families to arrange for children to be married to ease the financial pressure of keeping them at home. The Zubin Foundation, which works to support marginalized ethnic minorities in Hong Kong, saw their helpline receive 1,438 calls during 2020, more than three times higher than the number of calls received the year before. A similar trend of increasing forced marriages has also emerged in Mauritania, where girls facing descent-based slavery are being pushed into marrying early as a means of economic survival amidst the pandemic.
In Qatar, some 2 million migrant workers make up about 95 per cent of the total labour force, sustained by the vast construction boom over the last decade ahead of the 2022 Fifa World Cup.
Unsafe working conditions
It is important to note that minorities and indigenous peoples across the globe are often over-represented in jobs that have been classified as ‘essential’ and ‘key’ during the pandemic. These are often those working on the frontline, such as doctors, nurses, cleaners, grocery shop staff, bus drivers and truck drivers, whose jobs cannot be conducted from home and require human interaction, thus leaving them more exposed to Covid-19. These workers are deemed necessary to the functioning of society during lockdowns and tough restrictions. Though they have always been essential to societies, cities and economies, the Covid-19 pandemic has underscored this reality. In the United Kingdom (UK), for example, the Office for National Statistics found that ethnic minorities, while comprising 11 per cent of the working population, made up one in five workers holding occupations with the highest potential exposure to Covid-19. In New York City in the US, meanwhile, people of colour make up three-quarters (75 per cent) of essential workers in the city.
The disproportionate representation of minorities in high-risk work in the US
While limiting the spread of Covid-19 in workplaces has been essential for the safe continuation of work, measures to ensure this have frequently been inadequate. This has been exemplified through the food production sector, particularly in Western countries. In the US, for example, many workers in the meat and poultry processing industry were infected with the virus. Ethnic minorities, particularly Black and Latino people and immigrants, are heavily represented in this sector. Even with the increased risk of infection, then President Donald Trump signed an executive order at the end of May 2020 requiring meat production plants to remain open. Trump’s order also offered additional measures to protect the industry from legal liability if more workers contracted the virus, while leaving workers vulnerable. Though companies began implementing fever checks and supplying surgical masks, many workers reported that physical distancing was not being implemented in factories, forcing them to continue working in crowded spaces.
The US’ largest online retailer, Amazon, also saw a sharp increase in demand for its products and delivery service from the start of the pandemic. With demand soaring, in the first weeks of the pandemic Amazon continued to operate at full capacity without implementing adequate protective measures, such as masks and social distancing, in its warehouses. With more than a quarter (26.5 per cent) of Amazon’s US workforce identifying as Black or African American in 2020, the large majority of whom are employed in its warehouses, Black workers were far more likely to be exposed to a higher risk of infection in the workplace.
Few protections for sanitation workers in South Asia
This increased risk of contracting the virus is a pressing concern for ethnic minorities and indigenous peoples, one that has not been adequately met nor addressed in many cases since the pandemic first emerged. For example, in India, jobs that Dalits and Adivasis have been forced to undertake for centuries – as cleaners, manual scavengers and waste pickers – have been considered essential services by the Indian government during the lockdown; yet the majority of these workers have not been given adequate PPE to protect themselves from contracting the virus. Similarly, in Pakistan, sanitation workers, who were deemed essential workers, mostly belong to religious minorities including Christians (who make up about 75 per cent of the workers) and Hindus. The work is poorly paid, considered low-status and high-risk in terms of potential Covid-19 infection, yet even when those doing it were recognized as essential workers they were not given adequate PPE to carry out their jobs. Moreover, most sanitation workers in South Asia come from a Dalit background, so the intersection of being a Dalit, poor and belonging to a religious minority means these workers are subjected to hate speech and exclusion on a daily basis – a situation even more acute for those who are also women.
Transport workers on the frontline
Though many countries saw travel restrictions imposed, transport staff on local, national and international routes have been essential workers throughout the pandemic. In many contexts, ethnic minorities make up a significant proportion of transport workers, and by being on the frontline – in many cases without PPE in the early weeks of the pandemic – they faced increased risk of contracting the virus. In the UK, for example, 30.5 per cent of Transport for London (TfL)’s workforce are ethnic minorities. In June 2020, TfL reported a concerning rise in spitting incidents against bus drivers during the pandemic, amounting to workplace violence and aggression, highlighting the types of risk faced by frontline workers. Moreover, the case of Belly Mujinga, a Black rail worker who died of Covid-19 after being spat at while on duty in March 2020, elucidates the risks facing frontline workers. In this case, a man told Mujinga that he was infected with Covid-19 before coughing and spitting at her. Whether racial discrimination was a factor in this case remains to be determined through an inquest into her death, which was announced in May 2021.
With over 90 per cent of global trade being moved by sea, some measures to mitigate the spread of Covid-19 implemented by states have severely impacted working conditions for maritime workers in the shipping sector. As a result of measures such as border closures, travel restrictions and grounded aircraft, it is estimated that between March and August 2020, only 25 per cent of normal crew changes took place. By June 2020, up to 200,000 seafarers were trapped on board ships, many of whom were serving on extended contracts. According to the International Transport Workers’ Federation, as a result some seafarers stayed onboard for more than a year, breaching the 11-month maximum set by international labour standards.
As emphasized by the International Maritime Organization (IMO), crew changes are essential because they ensure compliance with international maritime regulations to protect the crew’s safety, health and welfare. Over a quarter of the world’s seafarers come from the Philippines, leaving them severely exposed to the effects of the pandemic on the global shipping industry. In 2019 alone, more than 375,000 Filipinos were deployed as seafarers, working on both cargo and cruise ships, channelling an estimated US$6.14 billion in remittances back home – a major contribution to the economy. Therefore, not only did these extended periods of time trapped at sea breach their contracts, but they also left many seafarers, particularly in the Philippines, jobless, waiting to be deployed and concerned about their households’ financial insecurity.
Gaps in social protection and safety nets
Many governments have introduced measures to mitigate the economic impact of the pandemic, either by developing new social protection schemes or expanding on existing ones. Many government interventions have focused on areas such as supporting businesses, employment retention, workplace safety and other measures to prevent social hardship. Other popular measures implemented by governments also include cash transfer, food aid and extension of social security schemes.
Throughout the current crisis, the narrative has focused on different countries’ approaches and their comparative success, rather than on the efficiency of these responses in addressing the burden on different groups within wider society. It is vital to acknowledge that exclusion and marginalization have long been associated with the welfare state, especially when examining the historic experiences of women, ethnic minorities, migrants and LGBTQ+ communities. However, the pandemic can also be an opportunity to realize social justice while protecting the most vulnerable. Therefore, assessing only the provision of these measures to minorities and indigenous peoples, and access to them, will not address the root causes of these inequalities. It is also crucial to take into account the inequitable access to housing, employment, food security and health care among minorities and indigenous peoples that pre-dated the pandemic and have contributed to the disproportionate impact on these communities.
This section focuses on the extent to which social protection measures associated with the pandemic have acknowledged the structural disadvantages that minorities and indigenous peoples face in their societies and economies: for example, over-representation in the informal economy, barriers to securing identification documents and limited access to the internet.
The question of eligibility
One factor in the effectiveness of social protection provision is the criteria determining eligibility for these benefits. One indicator of this is the extent to which informal employment is recognized and included, since people with disabilities, indigenous peoples, minorities and migrants are over-represented in this sector. While many of the job retention schemes have widely supported those working in the regulated economy, very few have covered workers in the informal economy. In many cases, enterprises and organizations are required to be registered in order to be eligible for wage subsidy. In addition, some countries only offered wage subsidies to specific sectors or enterprises, as was the case in Thailand, Botswana, Cambodia and Bangladesh. Many job retention schemes are found to exclude some members of minorities and indigenous peoples because of their failure to target workers in the informal economy. As a result, workers in the informal sector have been left vulnerable to destitution or exposed to unsafe and increasingly exploitative working conditions.
On the other hand, measures to mitigate economic hardship, such as cash transfers, social benefits and food aid, have been designed to target vulnerable populations and groups including informal workers, the self-employed, refugees, people living in rural areas and returned migrant workers. In addition to these targeted measures, there has been an attempt to include vulnerable groups in mainstream responses to the crisis through the relaxation of eligibility requirements to access benefits. Nevertheless, many governments have failed to target those most in need of support.
Ethnicity, citizenship and migration status have been widely used to shape eligibility for services even before the pandemic. Among the groups that have historically faced institutional discrimination in accessing social protection are stateless people and migrants, especially those who are undocumented. This discrimination has persisted throughout the pandemic. Some governments continued to exclude non-citizens from social security benefits, such as those of Iraq, Jordan and Spain. In South Africa, for example, while the stimulus package rolled out to provide social relief grants to unemployed workers during the pandemic was extended to include migrants and refugees, some 4 million undocumented migrants in the country were not eligible for this support. By contrast, among the most celebrated initiatives in promoting equality are those that extended unemployment benefits to include undocumented migrants, as in the case of California’s Disaster Relief Fund and Portugal’s regularization programme.
Domestic workers are another group who, having historically suffered from extremely limited social and labour protection, have again been excluded from social protection measures associated with the pandemic. Indigenous and migrant women are highly vulnerable to labour exploitation in the context of domestic work, especially in Asia and Latin America. In Latin America, domestic workers, especially those dependent on daily labour, have faced limited access to measures such as unemployment insurance, redundancy payments and sick leave. Although there have been some initiatives that identify and support domestic workers in Costa Rica and Argentina, where cash assistance was provided to this group, there is still a pressing need for this to be extended to address other immediate needs and protect domestic workers from slavery-like practices: for instance, through protections from wage theft and violence, and guaranteed access to public health information.
While extending eligibility to include vulnerable groups is welcome, on its own it is insufficient if the broader social and economic disadvantages they face are not also taken into account. Policy design should also address questions of sufficiency and sustainability. One indicator of this is whether welfare schemes provide adequate compensation or minimum thresholds to sustain a decent income for low-wage workers. This can readily be assessed in the case of cash transfer, since it is one of the most common measures used to target vulnerable groups: although governments have rolled out extensive cash transfer programmes in response to the pandemic, they have been widely regarded as inadequate, with countries such as Chile, Pakistan and South Africa providing packages below their national poverty lines. As a result, many members of minorities and indigenous peoples have faced increased pressure during the pandemic to work in unsafe and unprotected working conditions to secure their incomes.
Exclusion and lack of visibility
Even when members of minorities and indigenous peoples are eligible, that does not necessarily guarantee their access to services. Not only has financial and social assistance failed in some instances to reach many of the most vulnerable, it has also contributed to creating further inequalities within these groups. In many instances, governments rely exclusively on official registries to identify those targeted with assistance – an approach that often risks excluding undocumented migrants, residents of informal settlements and members of other communities on the margins of their societies.
In Bangladesh, for example, although the government has planned to widen the existing social safety net to cover low-income and marginalized groups, some minorities and indigenous peoples have received little support. According to a rapid assessment conducted by the Kapaeeng Foundation on the impact of Covid-19 on indigenous and tribal peoples in Bangladesh, only 2 per cent of the Rakhine community in Cox’s Bazar and 10 per cent of Maal Pahari received relief provided by the government. The same assessment showed that while some support was provided to minorities and indigenous peoples by NGOs, this was still not sufficient for them to meet their essential needs.
This failure to reach those most in need is clearly illustrated in the case of workers occupying what have historically been regarded as low-skilled jobs and those associated with inferior social status. This has shaped the experiences of many minorities and indigenous peoples who are disproportionately represented in cleaning, sanitation and domestic work in many parts of the world. A survey conducted by WaterAid found that, despite their vulnerability, sanitation workers in Bangladesh, India, Nepal and Pakistan have limited access to the measures introduced in response to the pandemic. Only half of the respondents in Nepal and Pakistan were able to access the social security aid for vulnerable populations, while only 5 per cent of respondents in India benefited from a direct cash transfer that was distributed as part of the Covid-specific emergency support led by the national government. These examples reflect the shortcomings of depending on pre-existing registries rather than crafting a universal response for distributing emergency assistance, given that the most marginalized communities are also the most likely to be left out.
One common precondition for being officially registered is the acquisition of identification documents, a situation that has often been instrumentalized to discriminate against minorities and indigenous peoples, even – in some cases – effectively criminalizing their presence in their country. In most countries, too, identification documents have been a prerequisite for accessing benefits during the pandemic. For example, in Thailand, while migrant workers are entitled to unemployment benefits in theory, in practice their access is limited as they must have a national ID number, a Thai bank account and supply other personal information, which many lack. Other barriers, such as limited access to the internet, can also prevent minorities, indigenous peoples and migrants from accessing benefits.
In South Africa, while social relief grants for the unemployed were extended to migrants and refugees, 4 million undocumented migrants were not eligible.
Other institutional barriersDiscrimination is not only tied to the divide between citizens and non-citizens but can also penalize minorities and indigenous peoples in their home countries. This can be illustrated in some of the experiences of domestic workers in Nepal, most of whom are women. Although the government has distributed food through local authorities during lockdown, some domestic workers were excluded as the municipality was only listing households in the locality, while most of the domestic workers do not own houses or are not locals from the community. This example underscores the multiple levels of discrimination that minority, indigenous and migrant women have faced throughout the pandemic.
Another factor influencing access to services among minorities and indigenous peoples is communication. The availability of accurate information has been at the centre of the fight against the pandemic, not only in public health discourse but also in relation to accessing social protection. Although there have been increasing efforts to employ minority and indigenous languages, especially in public health messaging, information on social protection measures has not always been communicated effectively. In some cases, communities have been formally included in welfare programmes, but have been largely unaware of these benefits because of poor communication. This reflects long-standing discrimination in accessing welfare, resulting in a lack of trust and inadequate support to marginalized groups.
This has been demonstrated in Kenya, for example, where a survey conducted in July and August 2020 by OHCHR and the National Coalition of Human Rights Defenders showed that while the large majority (90 per cent) of indigenous respondents acknowledged receiving information on Covid-19 preventive measures, less than a third (31 per cent) had received information regarding economic assistance packages. Furthermore, in India, according to a survey among migrant workers in the construction sector published by the Global Fund to End Modern Slavery in August 2020, of those who reported not having received any form of assistance during the pandemic, 58 per cent were unaware of the welfare schemes and benefits they were entitled to receive, while a further 27 per cent were unable to secure benefits despite having the necessary documents.
Conclusions
In order to address inequalities in responding to the pandemic, the deeper structural barriers affecting minorities, indigenous peoples and migrants must be overcome by granting universal access to Covid-19-related social benefits, without caveats or exceptions on the basis of citizenship or other official documentation. It is also imperative to address the misinformation associated with the pandemic in general by providing accessible channels of communication with clear guidance on benefits and measures available for workers and individuals to protect themselves.
The pandemic has highlighted long-standing protection gaps for millions of marginalized workers, forcing some governments belatedly to implement stronger rights and regulations to prevent abuses such as arbitrary dismissal or wage theft. The current crisis is an opportunity to dismantle structural inequalities and reconfigure societies towards more inclusive, rights-based labour models. This means recognizing the complexities and the multiple forms of discrimination that minorities and indigenous peoples face in the world of work and how these, in turn, intersect with gender, socio-economic status and disability. An essential first step in realizing this vision, however, is ensuring that members of marginalized communities are themselves allowed to contribute to the decisions affecting their livelihoods.
In this spirit, anti-discrimination efforts should centre on minorities and indigenous peoples as subjects and recognize their agency in driving change. One promising example of community engagement comes from New Zealand, where the government provided funding for a Māori business needs assessment with additional funding to allow Te Arawhiti (the Office for Māori Crown Relations) to work with iwi (Māori social units) to develop their own community responses to the pandemic. The pandemic has also witnessed many acts of solidarity, where communities have organized to cross lines of class, race, ethnicity and religion, as illustrated by the proliferation of mutual aid groups in many parts of the world. In the UK, for example, mutual aid groups have not only provided valuable support to elderly people, people with disabilities and other groups, but have also played an active role in campaigning for workers’ rights, especially workers in non-standard jobs and those excluded from government support. Many of these networks can be strengthened and used for different community mobilization and outreach projects. These structures can be useful, for example, in the efforts to support Covid-19 vaccine uptake and improve communication around vaccination campaigns.
Many members of minority and indigenous communities were already economically disadvantaged prior to the emergence of Covid-19, but the pandemic and the resultant economic crisis have exacerbated these inequities. Many from these communities have not only suffered job loss and reduced income, but have also faced an increased risk of exploitation and forced labour. Furthermore, social protection measures associated with the pandemic have the capacity to either address these impacts or worsen already existing inequalities. While there is some evidence of good practices in responding to the economic consequences of the pandemic, many of these measures have still failed to address the disproportionate impact on minorities and indigenous peoples.
At the end of 2019, on the eve of the pandemic, the global effort to achieve the UN Sustainable Development Goals (SDGs) was already off track. This unprecedented crisis is reversing decades of progress on poverty reduction and is deepening inequalities that are leaving minorities and indigenous peoples yet further behind. It is therefore critical that governments, businesses and civil society organizations act in a manner that ensures minorities and indigenous peoples can enjoy their social and economic rights.
Recommendations
- Recognize the complex social and economic barriers facing minorities and indigenous peoples in accessing secure, dignified work and welfare support: Policy-makers should ensure that any programmes or assistance are rolled out with a clear understanding of the specific challenges that different communities face. This means going beyond discrete or timebound responses that focus on a specific issue, to address instead the underlying discrimination they face.
- Remove citizenship requirements, exclusive eligibility criteria and other administrative barriers that bar marginalized groups from accessing benefits: In responding to the unprecedented crisis of the pandemic, social protection measures should move away from these and other constraints to ensure universal access for all members of society. Otherwise there is a danger that welfare may be distributed unevenly, further reinforcing existing inequalities.
- Ensure safe and non-exploitative working conditions for workers, particularly in informal or poorly paid sectors where labour rights are often non-existent or unenforced: This requires strengthening protections for workers not only through better laws and regulations, but also by enhancing mechanisms of accountability and remedies. Furthermore, during the pandemic, guarantees around PPE provision, social distancing and paid sick leave are crucial, especially for frontline and essential workers who are disproportionately from minorities and indigenous peoples.
- Uphold workers’ rights in the face of abuse and coercion, ensuring that victims of exploitation and other human rights violations can easily access justice: As unethical and even illegal business practices have increased during the pandemic, enabled by the precarious situation of many workers facing destitution or deportation, it is more important than ever that governments and businesses ensure workers are paid the wages and benefits owed to them. Measures should be put in place to disincentivize wage theft, arbitrary dismissal and other negative practices.
- Develop a clear evidence base on how ethnicity, religion and potential language barriers create barriers to accessing social welfare and other protections: One important element in this is the responsible collection and analysis of disaggregated data on financial assistance, unemployment and other indicators to better understand who is being left behind. This will help guide more targeted, inclusive labour protections and relief programmes that reach minority, indigenous and migrant communities, thus ensuring no one is left behind.
*This chapter draws on the findings of a rapid analysis project that collected and examined data from five regions: Asia and the Pacific, Europe, Africa, the Americas and the Middle East. This assessment was complemented by semi-structured interviews with over 30 non-governmental stakeholders. More information is available here.
Photo: Former Amazon employee, Christian Smalls, stands with fellow demonstrators during a protest outside of an Amazon warehouse as the outbreak of the coronavirus disease (Covid-19) continues in the Staten Island borough of New York U.S. Credit: REUTERS/Lucas Jackson.
-
By Sridhar Venkatapuram
The announcement by the World Health Organization (WHO) in January 2020 of a new and harmful infectious disease rightly raised the alarm among minorities and indigenous peoples around the world. Their concern, subsequently borne out by the disproportionate impact on these groups, was driven by a number of factors.
Alongside the endemic poor health these communities frequently face, they are also more exposed to harmful ‘risk factors’ (such as inadequate housing or hazardous employment) than the surrounding majority populations, further compounded by unemployment, discrimination and destitution. Besides often being more biologically susceptible to illness because of co-morbidities and poor health, they are also typically less able to access health care even in contexts where this is in principle universally available. At the same time, they are also overly represented in dangerous or insecure work that carries with it higher levels of personal risk, particularly during a pandemic, with many frontline jobs in areas such as nursing, delivery services and public transport occupied by members of non-majority populations. This complex range of factors meant that, long before the pandemic, health outcomes were significantly poorer for minorities and indigenous peoples – a reality that the pandemic has further reinforced.
Previous pandemics, most notably HIV/AIDS, have proved especially devastating to minorities, indigenous peoples and other socially-excluded groups. Notwithstanding the unprecedented scale of the current crisis, Covid-19 is only the latest in a long series of infectious epidemics and outbreaks, from tuberculosis and malaria to cholera and seasonal Lassa fever, that have been borne disproportionately by those on the margins of their societies. Even in wealthy countries where fatal infectious disease is rare, the impacts of the 2009 H1N1 pandemic on indigenous peoples in Canada and New Zealand, for example, revealed how the impacts of sudden health crises can be experienced very unevenly. In Canada, the division of roles and responsibilities between federal, provincial and territorial governments was not clear and produced jurisdictional disputes regarding funding as well as delays in decision-making for the provision of services. That Canadian experience shows how even the most well-resourced countries could be incapable or negligent in mounting a speedy, relevant and effective response to protect their minority and indigenous populations.
But the devastating impacts of epidemics for some minorities and indigenous peoples go back centuries, involving the intertwined spread of harmful viruses alongside colonial domination, land grabbing and, in some cases, acute depopulation and genocide. Based on this painful history, and more recent experiences of the SARS and H1N1 outbreaks, communities such as the Māori in New Zealand, the Cherokee Nation in the United States (US), and indigenous peoples in South America quickly took action and moved to protect their vulnerable. This also signalled to minorities and indigenous peoples elsewhere around the world the need to prepare. And, sadly, the fears of those who were raising the alarm early in 2020 have largely been borne out.
In many countries, minorities, indigenous peoples and other socially marginalized groups have been affected by higher levels of infection and mortality, from African Americans in the US to migrant workers in Southeast Asia. In the United Kingdom (UK), ‘while blacks are more than four times more likely to die from Covid-19, individuals of Bangladeshi, Pakistani, Chinese and mixed ethnic groups are about 1.8 times more likely to die from the pandemic’. At the same time, they are also facing greater barriers to accessing testing and care, a reality that is not adequately recognized when data is not disaggregated or is incomplete. Finally, as lockdown policies and other restrictions are often felt disproportionately by these communities, given their concentration in informal sector employment, the consequences can further deepen poverty and have negative health effects as a result of inadequate nutrition, evictions and other factors.
While the pandemic has brought greater attention to long-standing disparities, the needs and experiences of minorities, indigenous peoples and other disadvantaged communities are still not being given sufficient visibility. Complex social realities have often been overlooked or misrepresented by media and policy-makers, with communities often stigmatized for high infection rates without an understanding of the factors contributing to the prevalence of Covid-19. In the UK, for instance, some commentators have sought to blame the spread of the virus among minorities on ‘behavioural’ issues or an alleged failure to observe restrictions, rather than acknowledge the underlying social issues that have driven these spikes, from overcrowded, multigenerational households to their greater exposure to high-risk occupations. This lack of attention to diversity and inequalities among different social groups, both locally and globally, has contributed to the prescription of ‘one size fits all’ public health strategies that, in some cases, may be exacerbating the vulnerability of certain communities. For example, in countries where lockdowns are imposed without social support programmes, those already in economically precarious circumstances are more likely to take on potentially harmful work such as food processing, hospital cleaning, burials and cremations.
Looking beyond the immediate impacts of the pandemic, this chapter also explores what is needed for minorities and indigenous peoples to emerge from this pandemic and how progress towards realizing their equal right to health can be achieved. At a fundamental level, achieving meaningful progress towards this will require addressing long-standing issues of structural injustice. That is, aside from addressing the immediate concerns, such as access to basic preventative resources and vaccines, deeper systemic problems need to be confronted – the persistence of deep-seated inequalities that are a central cause of endemic ill-health among marginalized communities.
In the UK, ‘while blacks are more than four times more likely to die from Covid-19, individuals of Bangladeshi, Pakistani, Chinese and mixed ethnic groups are about 1.8 times more likely to die from the pandemic’.
Going beyond equity for minorities and indigenous peoples
One dominant public policy paradigm that continues to disadvantage minorities and indigenous peoples is the commonly accepted emphasis on utilitarian targets that aim to achieve ‘the greatest amount of good for the greatest number’ – a seemingly sensible proposition that can have the perverse effect of leaving the most excluded even further behind. For example, one of the identified failures of the United Nations (UN) Millennium Development Goals (MDG) agenda, running between 2000 and 2015, was that countries and international institutions focused exclusively on reaching the national targets while disregarding who, within a population, was experiencing or receiving the health and development benefits. It was the headline numbers that mattered most. Minorities and indigenous peoples, among the worst-off groups and individuals in many societies, were often neglected in the MDG efforts because it was easier and cheaper to reach larger numbers of better-off people and produce outcomes among them than among those who are marginalized – socially, physically or otherwise. The ethos of achieving targets in the face of global public scrutiny motivated a logic of maximizing efficiency over equity. As a result, social inequalities worsened in many places because those who were already somewhat well-off improved their health and lives even more. However, few would advocate for ‘equalizing down’ those with better outcomes, especially in terms of health. In contrast to maximizing cases, ‘equalizing up’ by giving priority to the worst off is a principle closely linked to improving the lives of minorities and indigenous peoples.
This was what the Sustainable Development Goals (SDG) agenda (2015–30) explicitly aimed to do and is reflected in the prominent tagline and ethical guiding principle of ‘Leave no one behind.’ While the SDG agenda is also structured towards achieving national and global targets, these must be achieved while also benefiting the worst off. However, in the first five years of the SDG era up to the beginning of the pandemic, in most countries little progress had been made. The pandemic and its multi-sectoral impacts are likely to put significant pressure on the ‘leave no one behind’ principle, if not render it meaningless. With national economies diminished and foreign assistance slashed, tentative successes in reducing extreme poverty in many countries have been erased, in the process reversing hard-won health achievements. It is unclear what will happen to the SDG agenda in the future, let alone the concern for equity and prioritizing those most behind. As pandemic recovery and rebuilding efforts intensify, governments and politicians will likely be aiming for as much economic growth as possible, even if it comes at the expense of environmental sustainability and social justice.
Yet this position is both unethical and counterproductive. On the one hand, the pandemic has made it harder than ever to ignore the structural violence and discrimination that have contributed, sometimes over hundreds of years, to the vulnerability of particular groups to ill-health and premature death. By extension, then, the societies that have created those harmful conditions now have a clear obligation to bring them to an end. At the same time, it has also brought to the forefront a realization that neglecting the health and well-being of one group exposes the rest of society, even the world, to the risk of a resurgence or a new threat taking hold. As the saying goes, ‘No one is safe until everyone is.’
Making the impact of Covid on minorities and indigenous peoples visible
As it stands, reliable data on infection rates, mortality levels and other indicators on Covid-19 are very difficult to achieve due to widespread under-reporting, lack of testing and other factors, including the reluctance of some governments to acknowledge the scale of their own problem. Though true across the world, this is particularly the case in countries where health systems and resources are already limited. In this context, it should not be surprising that, as with other health problems, data about the impact of Covid-19 on minorities and indigenous peoples is even patchier than what is currently available for the general populations. While in some richer countries such as the UK and the US, where health data is already disaggregated to some extent and communities have some protections in place, there is at least a partial picture of the impact on minorities and indigenous peoples. By contrast, in the Global South very little is known about how they are being affected. Nevertheless, extrapolating from the disparities where data is available, and widespread reports by human rights groups concerning lack of access to testing, health care or social welfare, it is likely that similar inequalities are at play. Indeed, in some countries there seems to be a clear practice of using the pandemic to scapegoat certain communities for the spread of infections. In India, for example, in the early weeks of the pandemic, Muslim individuals and groups were accused of spreading the virus.
Most of the research and reporting on the Global South has been about the population in general – how lockdown policies have impacted livelihoods, how infrastructure is being overwhelmed and the lack of vaccines – but with little discussion on the specific situation of minorities and indigenous peoples. There are some exceptions, however, that appear to highlight the disproportionate burden of the virus on these communities. For example, Brazilian researchers have reported that, while incidents among indigenous peoples are still under-reported, true mortality levels appear to be more than double those of non-indigenous Brazilians, with illegal mining, deforestation and land grabbing playing a key role in driving up infections. Other studies have identified lack of access to clean water or sanitation, communal living and proximity to urban centres as grave risk factors for indigenous peoples.
One dimension of the pandemic has been that the social distancing policies implemented to contain infections have been affecting minority and indigenous communities in very distinct ways. For a variety of reasons, many countries chose to respond to the pandemic by implementing radical physical distancing policies, such as nationwide stay-at-home orders. In richer countries, it was soon clear that in order for most people to be able to stay at home for extended periods of time, certain others would have to continue working outside their homes and provide a range of essential services – including health care, education, food, security, sanitation, transportation and other roles – to the rest of the population. A large proportion of those undertaking these vital but generally low-paid occupations were members of minority and indigenous communities, effectively risking their own health in order for the majority populations to be protected from the virus.
In the Global South, however, the standard lockdown approach had different dynamics. It was wholly implausible to expect millions living in urban settlements to practise social distancing and be able to work from home. It was similarly impractical to expect various pastoral or nomadic communities to comply with instructions meant for people with fixed and self-contained housing. Nevertheless, for these populations, failing to adhere to lockdown restrictions often meant being harassed or penalized for breaking the law. At the same time, those individuals who could not work from home and who were not regarded as essential workers – those paid hourly wages and working in entertainment, restaurants or street vending – had their livelihoods suddenly cut off. Again, workers in these kinds of insecure, low-paying jobs also belong disproportionately to marginalized groups and were also often unable to access welfare or support. The consequent negative impact on health and well-being, such as malnutrition and stunted growth, is only now being recognized. For example, in addition to the direct threat of Covid-19 itself, people living in refugee camps and migrant settlements worldwide, who are heavily dependent on international organizations and host governments for basic necessities, have faced increased hunger, intimate partner violence and morbidity as host and donor governments have chosen to focus on their own national populations instead.
The lack of internationally available and reliable information on the impact of Covid-19 on minorities and indigenous peoples is surely due in part to the wider absence of data collection facilities in the Global South. But it can also arise as a result of political indifference or a conscious desire to conceal. The problem of missing data does and will have enormous consequences for the future right to health and the health outcomes of minorities and indigenous peoples long after the pandemic has receded. In particular, the non-recognition or obfuscation of acute suffering and preventable deaths within these communities, through the absence or denial of official statistics, is one form of oppression. A remedy cannot be pursued if official or visible sources of data do not identify or recognize the problem. This is why calls for disaggregated data showing the specific outcomes for minorities, indigenous peoples and other disadvantaged social groups are so important. Given that the large majority of countries signed up to collect and publish disaggregated data when they signed on to the SDG agenda, this would simply require them to follow through on their commitments.
Impact reflects long-standing deprivations and relative inequalities
While large datasets or comprehensive evaluations may not be available, a growing variety of other sources document the experience of marginalized groups such as migrants and refugees as well as minorities and indigenous peoples. Drawing on disparate sources ranging from research publications and grey academic literature to news reports and social media, it is clear that protecting these communities from the health risks and associated social impacts of the pandemic requires some urgent interventions, whether it be access to information and personal protective equipment (PPE) to prevent infections or equitable provision of testing and vaccines.
But addressing the vulnerability of minorities and indigenous peoples to Covid-19 also requires addressing long-standing issues of discrimination. This means expanding our frameworks and reasoning beyond access to or redistribution of resources to tackle broader injustices, including structural racism. This matters very specifically in relation to the current pandemic, as well as poor health outcomes in general, because so often the solutions are framed in terms of access to goods and services such as health care or vaccines. To put it simply, securing access to vaccines and other resources is profoundly important for minorities and indigenous peoples, but the wider societal issues that have left them persistently vulnerable to acute health threats (HIV/AIDS, SARS, H1N1, Zika, Covid-19), as well as endemic levels of chronic diseases, injuries and impairments, must also be addressed. Improving health capabilities and building resilience among these marginalized communities to protect themselves and future generations from the next pandemic, as well as other diseases, require that underlying inequalities are effectively addressed.
In the US, data released by the CDC showed that between February and July 2020, 78 per cent of Covid-19 deaths of people under 21 years of age were of minorities or indigenous peoples.
Structural racism and public health – minorities, indigenous peoples and Covid-19
There is very little debate or controversy so far about which countries have been most severely affected by the pandemic in terms of deaths. It is also not controversial that the impacts of both the virus itself and policy responses are not randomly or evenly affecting all individuals or groups in societies. It is also accepted that in severely affected countries, minorities and indigenous peoples have been disproportionately affected compared to majority populations. For example, ‘Black and Latinx people and Indigenous Americans are roughly three times as likely to be hospitalized and twice as likely to die from Covid-19 as are white, non-Hispanic people in the United States.’ There is, however, much debate about why these groups have been so adversely affected.
One way to understand the controversy is to recognize that there are two competing kinds of explanations. Some professions seek to explain why more members of minorities and indigenous peoples are getting sick and dying by examining biological causes, particularly genetic traits specific to minority and indigenous populations. Because Covid-19 is a disease and biological functioning is a natural process, they seek a natural science explanation about why biology is functioning poorly or fails. In contrast, others seek to explain disproportionate exposure to the virus, as well as pre-existing biological vulnerabilities, in terms of the effects of social conditions certain communities experience daily and how they accumulate over the life course.
Those looking beyond biomedical causes have been able to show how minorities and indigenous peoples are being disproportionately affected by Covid-19 deaths and disease in Canada, the UK, the US and some other wealthy economies. For example, in the US, data released by the Centers for Disease Control and Prevention (CDC) showed that between February and July 2020, 78 per cent of Covid-19 deaths of people under 21 years of age were of minorities or indigenous peoples. Meanwhile, researchers in the UK observed that ‘deaths from Covid-19 among people from ethnic minorities are two to four times higher than in the white majority population’ – disparities they attributed in part to ‘comorbidities, overcrowded housing, income inequality and occupational risk’.
While racism has always underscored health inequalities in societies, contemporary activist movements, particularly the social protest movement of Black Lives Matter and related campaigns to decolonize global health, aim to show that the health inequalities that have become visible during the pandemic are not accidental or in some way natural events, but rather the reflection of persistent and pervasive efforts of domination and exclusion. The importance of this wider awareness is that previously the emphasis has been on the material deprivation associated with the status of belonging to a minority or indigenous community as the key factor determining poor health. Now structural racism is being identified, not only as a primary cause of deep-seated material deprivation, but also as an independent cause of vulnerability and harm. There seems to be a growing public understanding that institutions worldwide have, through structural racism, perpetrated violence against minorities and indigenous peoples – including through national public health systems. These are long-standing global problems that are evident at a global level between richer and poorer countries, but also evident within countries between the dominant and the marginalized.
Beyond the science – designing accessible and appropriate responses
In light of the disparate impacts of the pandemic on different social groups, some governments, organizations and social movements are seeing the current crisis as an opportunity to address long-standing structural injustices. These efforts have often been led by minorities and indigenous peoples as they have mobilized in response to the disproportionate impacts of the pandemic among their populations. However, despite being among the worst affected, they have frequently been disregarded by policies and programmes that are designed first and foremost with majority populations in mind.
Lockdown rules, welfare support programmes, new public health legislation, testing facilities and other services are all modelled on a particular vision of a citizen or subject. For example, a drive-through testing facility may be accessible to large numbers of people in a city, but inaccessible to those who do not have cars. Preventing any further erosion of health outcomes and capabilities among minorities and indigenous peoples in light of the pandemic will require concerted and specifically designed efforts. It cannot be expected that the acute vulnerability or harms that certain communities face will be adequately improved through yet more generalized approaches to recovery and rebuilding. The recent history of the MDG era demonstrates that minorities, indigenous peoples and other groups can continue to be excluded even when the majority populations are faring well.
Many governments have sought to justify their policies as ‘following the science’. But such an evidence-based approach would mean following epidemiological analyses which show the prevalence of risk and disease is higher among minorities and indigenous peoples. Given that this is an infectious disease epidemic, this should mean that efforts are targeted to reduce the risk of the most vulnerable and mitigate the further spread of the virus within these communities. Instead, public acknowledgement of the acute impacts on certain population groups, particularly minorities and indigenous peoples, has been minimal.
Yet when communities have been allowed to play a central role through meaningful engagement, outcomes have often been greatly improved, as demonstrated by community-led health strategies employed by indigenous peoples in Australia and Canada. Such examples show how appropriately implemented community participation can jointly achieve epidemiological goals and realize human rights principles. Such efforts also move away from viewing these communities as passive subjects with acute vulnerability to being active agents protecting and expanding their capabilities to be healthy over the longer term.
Where next?
The pandemic has made it glaringly obvious that to be healthy and stay healthy is not just a matter of having access to health care when you fall ill. Good health requires a whole range of physical, social, economic and other conditions at the household and community levels, as well as nationally and globally. In richer countries in particular, it was soon clear that protecting oneself and loved ones from potentially fatal infections required being able to stay at home for long periods of time. This, in turn, required a large number of further capabilities: having sufficient public health information about the risks in a language that is comprehensible; a safe home with sufficient space to be indoors for days and weeks; associated equipment such as a computer, internet and phone; and access to cash or credit to buy groceries. From this perspective, it is evident that Covid-19 deaths and disease follow the patterns of how health capabilities are usually distributed in a society. The situation of minorities and indigenous peoples can also be understood in terms of health capabilities, rather than just in terms of access to health care. Previously, high levels of poor health and co-morbidities made them more biologically vulnerable to infections. The surrounding conditions further constrained their abilities to protect themselves: for example, communities may not speak the dominant language in which public health information is provided, or lack ID cards to access public facilities.
Policies therefore need to go beyond health care or public health. However, addressing the deeply entrenched social dynamics and relations that help perpetuate domination and marginalization requires a wide range of different efforts, including rights-based advocacy and collective action, particularly within and across communities, to address structural injustice. This means mobilizing for the protection of not only the human right to health but all human rights of minorities and indigenous peoples. Where societies protect all the human rights of all individuals and communities, especially those who are most vulnerable to ill-health, all individuals and communities will enjoy better health outcomes and be more resilient against threats such as pandemics.
Preventing the next pandemic?
While some may be focused on recovery and rebuilding from the current pandemic, there is an understandable interest in preventing the next pandemic or other health emergency. The next major infectious disease outbreak or pandemic will be different in some ways. But it will not be surprising when it happens as the WHO and other organizations are constantly identifying and monitoring outbreaks that they consider could be sources of future epidemics. Indeed, many of those potentially dangerous viruses arise from situations where there is a human role. Massive deforestation exposes new organisms to humans, poor human–animal interactions can produce new organisms, rising temperatures may expand zones of existing epidemics, and so forth. Addressing the potential sources of new and resurgent epidemic threats will require a range of cooperative actions from the local to the global. World leaders have recently called for an international pandemic treaty in order to better alert countries, create better systems for data collection and distribution of relevant goods, and, importantly, address the sources of global health threats.
However, it remains to be seen whether global efforts to avert the next major health crisis will focus on the crucial role of structural racism towards minorities, indigenous peoples and other marginalized communities. Just as national policies have focused on policies for the general public, international agreements will likely focus on institutions with various functions. But while we know that access to goods such as masks or hand sanitizers, and health care, including testing, are all important, they too are only partial components of health resilience. The scope of pandemic prevention must be human focused, and help individuals promote their abilities to prevent infections in themselves, their families and communities. And, importantly, preventing future epidemics means promoting health now, so that populations are as healthy as they can be when a new health threat emerges.
Failing to recognize the crucial role that social exclusion and discrimination play in pandemics and other health emergencies, as well as the everyday functioning of health systems, means that next time infections will once again spread among the most disadvantaged communities. There is a real possibility that without sufficient supply and distribution of vaccines in the Global South, Covid-19 could persist indefinitely, potentially enabling the emergence of more harmful variants of the virus and then a resurgence in infections across the entire global population. All of this is to say that addressing the underlying drivers of poor health for minorities, indigenous peoples and other marginalized groups is crucial to addressing the entire human population’s vulnerability to the next global health threat.
The principles that underpin the right to health and other human rights more generally for minorities and indigenous peoples continue to have salience during the pandemic and are crucial for recovery. First, the right to health encompasses more than health care, and includes supportive conditions that protect and expand the capabilities of individuals and communities to be healthy over the long term. Second, minorities and indigenous peoples have a right to non-discrimination in accessing and experiencing health care, as well as public health policies. And, third, the right to participate in health-related decision-making at the personal and policy level must be respected and realized. Fourth, the right to protection of identity must be respected, because many communities have beliefs and practices related to health and well-being that are central to their personal and group identities. Addressing the acute vulnerabilities of minorities and indigenous peoples is a prerequisite for ending this pandemic for all, as well as for protecting the health of all societies in the future.
Recommendations
- Refocus data collection and disaggregation efforts to ensure the situations of the most excluded are not concealed or overlooked: In line with the promise of the SDGs to ‘leave no one behind’, it is vital that the specific outcomes of minorities and indigenous peoples are adequately captured in official data and targets. These systems, while urgently needed during the pandemic, should be maintained after recovery to assess and respond to the incidence of other health inequalities among communities.
- Ensure that public health strategies reflect the specific social realities of minorities and indigenous peoples, with measures in place to ensure their rights are protected: The ‘one size fits all’ approach to managing the pandemic has in some cases placed marginalized communities at greater risk by failing to recognize the precarious nature of their livelihoods and the lack of an economic support net to weather the crisis. However, the imposition of standardized medical policies predates Covid-19 and is likely to continue without sustained efforts to design policies that are accessible and appropriate.
- Involve minorities and indigenous peoples in the design of public health responses to ensure their relevance and effectiveness: Human rights-based approaches to public health require meaningful participation by community representatives in the design and implementation of any strategies directed towards those communities. This includes groups that may be marginalized within minority and indigenous communities, including women, persons with disabilities, older persons and LGBTQ+ persons.
- Address the fundamental role of structural racism in perpetuating health inequalities: While disparities in outcomes have often been framed in material terms, acknowledging the association with higher poverty levels among some communities, there has been less recognition of the roles that racism and discrimination have played in determining these gaps. Public health should therefore embrace an approach grounded in principles of social justice and anti-racism that includes a wide range of human rights.
- Promote a rights-based pandemic recovery that addresses not only inequities around Covid-19, but also other health challenges: The disproportionate burden borne by minorities and indigenous peoples during the current crisis illustrates historic, longstanding inequities that will remain in place long after the end of the pandemic. These must be addressed to ensure lasting equity and resilience not only for these communities but also for societies as a whole.
Photo: Indigenous Muruwari elder Rita Wright, a member of the ‘Stolen Generations’, is seen at home with her son Dean Wright, who is ill with kidney failure, in Sydney, Australia, January 19, 2021. Picture taken January 19, 2021. Credit: REUTERS/Alamy.
Universal health
Ensure the right to health for all, including full and equitable access to care, is a priority not only during the pandemic but also a central element in the global recovery: The disproportionate impact of Covid-19 on minorities and indigenous peoples has highlighted longstanding health disparities that are likely to remain in place without sustained action to address them. Though there has been widespread recognition that the burden of Covid-19 has been borne heavily by minorities, indigenous peoples and migrants, the current crisis has simply exacerbated a reality that has often been overlooked – the immense inequities around health provision, nutrition, living conditions and other determinants that have left them more exposed to chronic illness, disease and death. These drivers have simply accelerated during the pandemic, resulting in higher infection and mortality rates among these groups. While it is vital that testing, treatment and vaccination are rolled out equitably across the world to target those communities most at risk from the virus, efforts should also focus on securing a long-term transformation of public health that ensures that no one is left behind. In the wake of Covid-19, it is impossible to ignore the profound exclusion of many populations from the right to health, and the dangers that this poses not only to the communities directly affected but the world as a whole.
- 01

Australia: The essential role of community action for First Nations people with disabilities during the pandemic
By June Riemer and Karen Soldatic Disability, chronic conditions and illness disproportionately impact on Australia’s First Nations peoples. According to a nationwide survey conducted by the Australian Bureau of Statistics in 2015, almost…
0 min read
- 02

Canada: Indigenous health governance during Covid-19
By Sean Hillier and Elias Chaccour At the start of the pandemic, there was widespread concern within Canada that the spread of Covid-19 would disproportionately impact Indigenous Peoples compared to the broader general public. Since…
0 min read
- 03

United States: For decades, Black Americans have been living through a public health crisis
By Menka Sandrasagren Long before the outbreak of Covid-19, a significant portion of the US population were already suffering from profound health inequalities. These disparities have been made worse by the effects of the virus and are…
1 min read
-
By June Riemer and Karen Soldatic
Disability, chronic conditions and illness disproportionately impact on Australia’s First Nations peoples. According to a nationwide survey conducted by the Australian Bureau of Statistics in 2015, almost a quarter of the estimated 523,200 Aboriginal and Torres Strait Islander population were living with disabilities, compared to only 17.5 per cent of non-Indigenous Australians.
However, First Nations people with disabilities live in a variety of geographical locations, including inner-city areas, regional towns and remote First Nations communities. As a result, access to appropriate disability support and services varies and is highly uneven.
This has meant that many First Nations people living with disabilities experience what is commonly referred to as double or triple disadvantage, due to long-standing experiences of racism, disablism and, at times, geographical location. The intersection of disability, Indigeneity and geographical location has therefore resulted in specific outcomes and impacts for First Nations communities during the long lockdowns and continued uncertainty brought on by Covid-19.
Most importantly, it has been the leadership role of First Nations communities, organizations and services that have sustained community members living with disabilities, keeping them safe, well and supported throughout the pandemic, thanks to their respectful decision-making and democratic safeguarding.
Closing First Nations communities: Rapid leadership and direction
Given the level of health vulnerability experienced by many First Nations community members, particularly with regard to chronic illness and disease, First Nations peoples across Australia rapidly ‘shut down’ access to outside residents, officials and non-essential staff and workers in response to the outbreak of Covid-19. This occurred prior to the national Australian government shutdown. The decision to close down external access to First Nations communities, particularly in rural and remote regions, was driven by Indigenous medical expertise within the First Nations community-controlled health sector. Despite being under-funded, with experts often stretched thin given the large areas they are required to cover and travel around, the swift response kept community members safe, many of whom are among those most susceptible to the worst impacts of the virus.
As a result, First Nations communities in Australia, unlike other Indigenous communities facing settler-colonial contexts, were able to maintain one of the lowest rates of community transmission across the country through these active strategies of Indigenous sovereignty and taking control of their lands. Yet this strategy of self-imposed community shutdown was highly contested by local and state authorities. For example, in some regions, government officials removed First Nations’ community blockades to enable ongoing access, even though there were no national protective safeguards in place at this time. Community members persisted and resisted local authorities’ demands, instead trusting in First Nations’ medical expertise and recommendations.
Access to PPE and support for vulnerable family members
For rural and remote First Nations residents living with disabilities or chronic illnesses, one of the core issues to emerge was the lack of access to appropriate personal protective equipment (PPE) and disability supports. It took extensive lobbying of government at both the state and federal levels* to access the necessary resources to protect disabled community members and members living with chronic, potentially life-threatening conditions. These measures were necessary to ensure that critical essential workers moving in and out of the community did not unwittingly contribute to transmission of the virus. The large distances between First Nations communities, and between these communities and core, essential health and medical services within rural and remote Australia, mean that the movement of essential workers from community to community creates heightened risk of coronavirus spread across vast regions. Thus, timely, readily available PPE was critical for First Nations members living with disabilities or chronic conditions.
Nevertheless, even with extensive pressure from First Nations disability advocacy groups, consideration of disabled community members was often absent from both the formal First Nations community health services and the mainstream disability response. Communities often relied on the goodwill of trusted volunteers and family members to take up personalized support roles in the absence of specialist paid disability support workers. Additionally, Aboriginal organizations such as First Peoples Disability Network also mobilized their local workers to step in and support those communities where critical disability supports needed to be maintained. Again, it was the self-organization of First Nations communities and agencies that protected First Nations community members living with disabilities or chronic conditions.
Access to essential goods and services: Food insecurity
One of the core issues faced by many members of the disability community in Australia was the lack of access to essential goods and services, especially in relation to sustaining high-quality nutrition. Working in partnership with the Muslim charity Al-Ihsan Foundation Australia, local staff from the First Peoples Disability Network identified residents with disabilities in need of food, water and other essential items. Extensive lists were created to establish national distribution of food parcels. This effort played a critical role in overcoming food shortages brought about by urban residents – themselves reacting to the panic buying in cities – travelling to regional and rural towns to purchase items in bulk.
This not only had the effect of depleting local stocks, but also resulted in additional costs for First Nations communities. Often, after driving 200 to 300 kilometres to regional supermarkets from remote towns and communities, First Nations community members would find shelves empty of stock, forcing them to make the same journey again a few days later with no guarantee food supplies would have been replenished. This resulted in many First Nations communities spending large sums on petrol and transport, a situation which would quickly have proved unsustainable. The partnership between Al-Ihsan Foundation Australia and the First Peoples Disability Network was absolutely critical in shoring up food security for residents in remote locations living with disabilities or chronic conditions during this fraught time.
Sovereignty, self-determination and justice: Black Lives Matter
Finally, the death of George Floyd in the city of Minneapolis in the United States galvanized Australia’s First Nations peoples into action. Even though the federal and state governments attempted to foil the national days of action and demonstrations by suggesting the possibility of mass community transmission as an outcome, and in some instances refraining from issuing or withdrawing permits to protest organizers, First Nations peoples and allies rallied in cities across the country. First Nations activists carefully crafted and monitored these protests across the country to protect community members and allies, particularly as some members had travelled from remote rural areas. These protests were in response to the ongoing injustices First Nations people experience with police and the rise of Indigenous deaths in custody, despite years of First Nations advocacy, activism and lobbying aiming to change the situation.
The struggle for sovereignty, self-determination and justice continued throughout the pandemic, and First Nations in Australia have remained at the forefront of campaigns for racial justice, respect and self-determination. The First Peoples Disability Network and collaborating organizations have been part of these campaigns, given the high rates of First Nations community members living with disabilities who have been incarcerated. They have been particularly active around the Royal Commission into Violence, Abuse, Neglect and Exploitation of People with Disability, undertaking extensive submissions. Their continued leadership in the midst of the current crisis is a testament to the essential leadership role of First Nations communities in ensuring their sovereignty and self-determination.
*Australia is a constitutional federation where there is a well-articulated division of responsibilities across federal and state governments, along with local governments. This creates a number of particular issues for First Nations peoples as their communities cut across multiple state borders and municipalities.
Photo: A painting by an Aboriginal sister telling the story of her younger sister with a disability and their mother, Australia. Courtesy of First Peoples Disability Network Australia.
-
By Sean Hillier and Elias Chaccour
At the start of the pandemic, there was widespread concern within Canada that the spread of Covid-19 would disproportionately impact Indigenous Peoples compared to the broader general public. Since European contact, Indigenous Peoples in Canada and around the world have been disproportionately impacted by pandemics, including smallpox, influenza, TB, HIV, HepC and H1N1.
Greater susceptibility to adverse health outcomes from infectious diseases is the result of an ongoing history of genocidal policies, either promoted or permitted by colonial structures, which actively marginalize Indigenous Peoples from basic rights such as health care infrastructure, clean drinking water and stable non-crowded housing, to name a few.
However, despite concern and predictions of the possible imminent collapse of Indigenous social systems in the face of a significant pandemic, many Indigenous communities in Canada are asserting their authority in managing and containing the virus, including creating their own public health orders, restricting travel through their territory, adapting ceremonies and intensifying Indigenous-specific and relevant public health campaigns. This phenomenon is being recognized as an expression of Indigenous self-governance and a continued assertion of sovereignty and nationhood. Indigenous nations and communities across Canada have implemented, to varying degrees, principles of Indigenous health governance, including nation-to-nation relationship-building and decision-making, self-government, self-determination, reciprocal accountability and meaningful community engagement. As a result, the overall impact on Indigenous communities has been less severe than on the general public in Canada.
Throughout the pandemic, Indigenous communities have established partnerships with national, provincial, territorial, regional and municipal health and social services agencies, and both Indigenous and non-Indigenous health care providers to mount an effective public health response. In addition to deploying Indigenous-specific and responsive testing and contact tracing campaigns, communities have worked to combat vaccine hesitancy by establishing culturally relevant communications strategies and Indigenous-led vaccine clinics that create an environment of safety and trust for their people. Indigenous nations have demonstrated that they are best equipped to respond effectively to their own people’s unique health needs through a community-specific approach: for example, by providing culturally sensitive information in Indigenous languages and respecting cultural practices.
Indigenous assertion of self-governance led to the effective deployment of vaccines, which caused Covid-19 cases in Indigenous communities to drop by more than 85 per cent between January and April 2021.
As the Canadian government secured millions of doses of Covid-19 vaccines, Indigenous leaders led a nation-to-nation lobbying campaign to apply pressure to the federal government to ensure they would be prioritized for vaccine access. As a result, the government of Canada declared Indigenous adults, including First Nations, Métis and Inuit, as a high-priority group and among the first groups to receive the vaccine. This was a significant development, given the long history of marginalization and sub-standard care afforded Indigenous Peoples in Canada, and was the result of relentless Indigenous advocacy and research on the urgent need to counteract the detrimental effects of colonization on Indigenous Peoples’ health – particularly in the face of a virus that posed severe risks to their communities.
However, while Indigenous leaders fought for access to vaccination, harmful and false tropes circulated throughout the country, fuelling concerns that vaccine hesitancy among Indigenous Peoples would hinder the overall pandemic response. This misconception does not stand up in the face of data suggesting that vaccine hesitancy was not more pronounced within Indigenous communities when compared to non-Indigenous communities. Much of this resulted from the effective health response and information campaigns mounted by Indigenous leaders and systems themselves, a testament to the success of Indigenous health governance in times of crisis.
Indigenous assertion of self-governance led to the effective deployment of vaccines, which caused Covid-19 cases in Indigenous communities to drop by more than 85 per cent between January and April 2021. Indigenous community actions and Indigenous health leadership created an atmosphere of trust that led to increased vaccination uptake among Indigenous Peoples, contributing to the decline in communities’ active cases and protecting them against future outbreaks. In May 2021, as the third wave of the pandemic raged across most of Canada, more than 50 per cent of Indigenous adults living in their communities had received at least one shot of a Covid-19 vaccine, a figure four times higher than that for the Canadian general adult population.
Indigenous communities and health care providers facilitated the successful uptake of vaccination by creating an environment that reflects the people’s cultural needs. For example, community vaccination clinics allow their members to participate in traditional ceremonies and medicines when they come to receive their vaccines, blending both Western and Indigenous perspectives. Community vaccination clinics were integrated within the shared social spaces of communities, where elders could take time to understand the Covid-19 vaccination process and then connect with one another in a safe and socially distanced way after receiving their injections.
Indigenous leadership in vaccination extended beyond their own reservations’ borders to reach their community members living in Canada’s towns and cities. While Indigenous People living in urban areas were similarly placed on government vaccine priority lists, ensuring adequate uptake required different strategies to reach and inoculate this population. For example, in Thunder Bay, Ontario, the Mattawa Indigenous tribal council servicing remote communities began running vaccination clinics aimed at vaccinating people hailing from their communities along with other Indigenous People in the core of the city. These clinics offered culturally safe services in Indigenous languages as well as transportation and childcare for those who required it. In Toronto, where Indigenous Peoples are more dispersed and difficult to reach, Indigenous health organizations, including Anishnawbe Health, have offered pop-up mobile vaccination clinics to reach those who are homeless and are most vulnerable during the pandemic.
All of this is a testament to the success of Indigenous Peoples’ assertion of health governance and sovereignty, and the successful nation-to-nation collaboration and partnerships between Indigenous leaders and governments at all levels. Indigenous nations, through their sovereignty, have clearly demonstrated through their response to the pandemic that they are highly proficient and capable of dealing with major health emergencies. In fact, they have been more effective than most communities in Canada, stemming the pandemic’s advance and promoting immunity among their citizens. This runs counter to widely held notions within Canadian society of Indigenous Peoples being unable to manage and run their own affairs without state oversight and surveillance. Indigenous communities’ success in administering vaccines to their people has even influenced vaccine distribution for non-Indigenous Canadians. Indigenous communities are now playing a vital role in expanding Covid-19 immunity to their neighbours. For example, the Saskatoon Tribal Council and the Prince Albert Grand Council are opening vaccine clinics that will serve Indigenous and non-Indigenous people. These clinics will also provide smudging ceremonies and will have staff who will help people navigate language barriers. These clinics actively dismantle the colonial legacies that led to a health care system rife with racism and barriers to accessing care for all marginalized communities. This assertion of health governance principles is essential for continued efficient health care delivery to Indigenous communities in Canada and for dismantling colonial structures that hamper all other marginalized people’s progress.
Photo: Residents, including Chief Wilfred King, far right, stand at a checkpoint restricting access to their community to slow the spread of coronavirus disease (Covid-19) in their remote First Nations community of Gull Bay, Ontario, Canada April 27, 2020. Picture taken April 27, 2020. Credit: Reuters/David Jackson.
-
By Menka Sandrasagren
Long before the outbreak of Covid-19, a significant portion of the US population were already suffering from profound health inequalities. These disparities have been made worse by the effects of the virus and are particularly pronounced along ethnic lines, with Black Americans more at risk than any other group due to their limited access to testing and treatment.
Furthermore, without substantive change to the country’s social and health systems, these inequalities are likely to continue once the pandemic is over. This is reflected in the fact that time and again, across a range of public health challenges from lead poisoning to tuberculosis, Black communities have been significantly worse affected than the white population.
One long-standing problem is the disproportionate number of Black Americans without health insurance: in 2019, on the eve of the pandemic, 11.4 per cent of Black people were uninsured, compared to 7.8 per cent of the white population, a rate close to 50 per cent higher. As insurance plays a major determining role in the ability of citizens to access health care, the large coverage gap is a significant factor in their poorer health outcomes. For example, Black Americans have the highest mortality rate for all cancers combined and almost twice the national average of infant deaths, at 11 infant deaths per 1,000 live births.
The devastating impact of inequalities on Black Americans has meant that, even in the supposed normality before the pandemic, they were living through a public health crisis. For example, a study by the academic Elizabeth Wrigley-Field, published in September 2020, estimated that pandemic-related mortality levels among the white population would need to rise by a factor of almost six to attain the same levels as those experienced by Black people outside the pandemic, leading to the startling conclusion that ‘even amid Covid-19, US White mortality is likely to be less than what US Blacks have experienced every year’.
In 2019, on the eve of the pandemic, 11.4 per cent of Black people were uninsured, compared to 7.8 per cent of the white population, a rate close to 50 per cent higher.
The biggest misconception early on in the pandemic was the myth that Covid-19 was the ‘Great Equalizer’, namely that the impacts of the virus would be felt equally among all demographics. The reality on the ground has been that the poor, the elderly and ethnic minorities have been disproportionately impacted by the virus. This is illustrated by the fact that the mortality rate up to 21 July 2020 from Covid-19 for Black Americans was 97.9 per 100,000, roughly double the rate of 46.6 per 100,000 for white Americans. One contributing factor in this is job precarity: for example, almost 40 per cent of Black workers are engaged in low-wage employment without paid sick leave. Other factors that have contributed to higher infection levels include the concentration of Black community members in segregated housing, often in unhealthy environments with limited access to health facilities.
All these determinants are closely associated with the Black American experience in the US and are determined by existing social systems that enable or prevent groups’ and individuals’ full enjoyment of the right to health. Without significant changes to the social and health systems of the country, there is a risk that the inequalities already exacerbated by Covid-19 will increase significantly. These changes need to have at their core the protection of human rights and human dignity, by ensuring that policies aimed at addressing the pandemic do so in a equitable and targeted manner. Instructions to self-isolate need to be met with actual financial support for workers and families if they are to be able to live without fear of dismissal. Access to broadband needs to be mainstreamed for children and workers working from home, to enable them to keep working and to prevent children from missing out on essential learning.
Whilst some changes are more intuitive, such as universal health coverage, paid family leave and paid sick leave, more ambitious policies also need to be put forward. Reducing food insecurity, ensuring adequate housing and strengthening mental health services are all necessary steps in mitigating the historical inequalities that Black Americans have faced. Only a complete transformation of the country’s inequitable social and health systems can prevent Covid-19 – and a host of other conditions, illnesses and hazards – from continuing to exacerbate the health inequalities that have so long existed between Black Americans and the white majority.
Photo: Health workers hold up Black Lives Matter signs as they demonstrate outside the a hospital in New York City to mark Juneteenth, commemorating the ending of slavery in the United States in 1865. Credit: Enrique Shore/Alamy Live News.
Housing and living conditions
Reduce underlying health inequalities through more equitable shelter and service provision for minorities, indigenous peoples and other marginalized communities: The pandemic has laid bare the disproportionate rates of death and disease borne by these groups as a result of inadequate housing and unsanitary conditions. The spread of Covid-19 has been driven by inequality, in particular the shortfalls in housing and living conditions that typically afflict marginalized groups, including minorities and indigenous peoples. Overcrowding and the absence of basic services, such as clean water and sanitation, have proven to be key factors in the spread of the virus in informal settlements, camps and other contexts. Even before the pandemic, these environments were exacting a heavy toll on health outcomes for minorities and indigenous peoples, contributing to lower life expectancy and above-average infection rates for communicable diseases such as tuberculosis. Better housing and service provision is therefore critical, not only to protect these groups from Covid-19 but also to boost resilience to other public health threats in future.
- 01

Ghana: For Liberian former refugees, Covid-19 has made life even more precarious
By Hamimu Masudi Upon his appointment as the Global Goodwill Ambassador for UNHCR (the UN Refugee Agency) in March 2021, Alphonso Davies, a young star at Bayern Munich Football Club and former child refugee, told reporters he wanted to…
0 min read
- 02

Greece: The role of youth and education in responding to the pandemic in Ritsona refugee camp
By Parwana Amiri When it was first built, Ritsona refugee camp – located in mainland Greece, just north of Athens – was meant to house around 900 people. Today, it provides accommodation to more than 3,000 refugees who have been…
1 min read
- 03

United Kingdom: For the London borough of Newham, Covid-19 is the latest chapter in a history of discrimination
By Zita Holbourne Newham, a deprived borough in East London with a high proportion of ethnic minority residents, has been one of the areas in the United Kingdom (UK) hardest hit by Covid-19. As a race equality and anti-austerity campaigner…
1 min read
-
By Hamimu Masudi
Upon his appointment as the Global Goodwill Ambassador for UNHCR (the UN Refugee Agency) in March 2021, Alphonso Davies, a young star at Bayern Munich Football Club and former child refugee, told reporters he wanted to use his platform to show how urgently refugees need support to survive and to thrive.
Alphonso’s message comes as no surprise. Born in Ghana’s Buduburam refugee camp, at the age of five he relocated to Canada under a resettlement programme, and developed into the football superstar that he is today. He recalled how his own parents had struggled to find food and water during their stay in Buduburam refugee camp.
But for the many thousands of child refugees like Alphonso who were not lucky enough to be accepted into a refugee resettlement programme, life in the camp is a constant challenge. It is crowded with traumatized people with limited access to food, health care and basic sanitation, and living conditions were already hazardous even before the pandemic. For many undocumented residents there is also a constant threat of deportation. Limited opportunities to earn an income have also forced large numbers into sex work and other areas of exploitation.
While the advent of Covid-19 and resultant lockdowns caught everyone unprepared, the impacts of the deteriorating situation have been magnified for those fending for themselves in Buduburam. Life for Liberian residents in the camp has long been precarious, particularly since Ghana withdrew recognition of their refugee status a decade ago, and with it the humanitarian aid they relied on. The only alternative to voluntarily repatriating back home to Liberia was to remain in Ghana under the vaguely defined status of a migrant, a path many chose over the insecurity of return – yet it has often left them in a limbo, with few protections or certainties, ever since.
In October 2020, the ‘Masks for Refugees by Refugees’ initiative in Ghana commissioned 40 refugee tailors and seamstresses to produce 35,000 masks to be distributed to refugees.
Because most worked in the informal sector, when Covid-19 struck large numbers of refugees and migrants lost their only sources of income as work possibilities vanished due to lockdowns and other restrictions. At the same time, like many other countries, Ghana adopted a range of policies that appeared to prioritize citizens over non-citizens, whose plight was often overlooked. In this context, former Liberian refugees, who were now only protected under restrictive rights to work, fell through the cracks, as the government enforced strict immigration laws and restricted freedom of movement, resulting in crackdowns on migrants and widespread loss of livelihoods. This has occurred in a broader context of fear and uncertainty for non-citizens in general amidst reported threats of deportation, closure of border points and restricted freedom of movement. As a result, some have been forced to flee from isolation centres and hesitated to seek health care and other social services.
Psychological needs are yet another area of concern for Ghana’s refugee populations. Frequently contending with the impacts of previous trauma, refugees and asylum seekers are often among those at greatest risk of mental health impacts of the pandemic, given the distinct challenges they face. This is reflected in the situation of refugee and migrant populations more broadly, as demonstrated by a global World Health Organization study that assessed the impact of Covid-19 on these groups in different countries and found elevated levels of depression, fear, anxiety and isolation. In most cases, there is little support to alleviate this burden. Although some refugees are being offered counselling, because of stigma, inattention to mental health issues and the refocusing of resources towards Covid-19 containment in many low-income countries, the full mental health impacts of the pandemic on Ghana’s refugee populations is impossible to gauge.
Recognizing the severe lack of personal protective equipment among refugee communities, in October 2020 UNHCR Ghana partnered with Abrantie, a Ghanaian fashion designer, to launch an initiative, ‘Masks for Refugees by Refugees’, which trains refugees to produce their own masks. The project, which commissioned 40 refugee tailors and seamstresses, was expected to produce about 35,000 masks to be distributed to refugees and members of host communities in Ghana, while creating livelihood opportunities for refugees – making a clear statement that, though often forgotten and excluded, refugee communities can rebuild, fend for themselves and even benefit host communities, if only given the chance.
Photo: A resident of Buduburam camp shows personal photos from 1990, when he arrived from Liberia to the camp. Credit: Delyan Todorov.
-
By Parwana Amiri
When it was first built, Ritsona refugee camp – located in mainland Greece, just north of Athens – was meant to house around 900 people. Today, it provides accommodation to more than 3,000 refugees who have been transferred here from the camps on the Greek islands. Most of them are considered vulnerable.
I am one of the new arrivals who left Moria camp on Lesvos, hoping that, here at Ritsona, we could find peace, dignity, education, health care and recreation: in short, the chance to lead a normal life and have all that a human being needs to do so. And, for a time, the situation did indeed improve for us, and we allowed ourselves to believe that we would regain some certainty and normality in our lives.
Unfortunately, very soon we found ourselves confronting a new problem: the Covid-19 pandemic. The official guidance on the most effective ways of protecting against infection is clear: ‘stay home, wear masks, keep a distance from others’. To do so, however, is almost impossible when you live in the midst of thousands of other people, crowded together in containers with eight or more people in each.
While throughout the world, the rule is to stay in isolation at home for a period of time, here the advice is just to stay in the camp. But in Ritsona, this does not make any sense. Here, people are physically close to each other every single moment. They have no information about what is going on in the world at large, nor about how they can protect themselves and their children from the disease. Unfortunately, the virus does not recognize any borders and treats everyone equally, even the refugees who face inequality in every other area of their lives.
For us, this camp is a communal home. While you have to stay at home, we have to live in the camp, where there is no guarantee of health or safety. We are in such close contact with each other that we could be considered links in a chain. If one of us gets the virus, in less than a week half of the camp will become ill. Hence, in the early days of the pandemic, some friends and I decided to organize an event with the residents of the camp to raise awareness and communicate information about the nature of the virus and its transmission.
As I had been a volunteer teacher in Moria for both children and adults, my experience there helped me to realize that change can be achieved in an educational space, where people come together to learn something new and better understand the realities of the world. We started with the youngest in the camp, making sure that they understood the instructions we had received from the camp’s doctor. I believe in the power of the young as they are generally better educated and able to learn faster than their parents. I was, therefore, convinced that they would readily appreciate the seriousness of the epidemic and explain it effectively to the adults in their family.
When I shared my idea with the community engagement team at the International Organization of Migration (IOM), they felt that an event of this sort would take a long time to prepare. Even so, I was convinced that it was worth trying and much better than doing nothing and passively accepting the approaching danger.
My first concern was to secure the engagement of the medical team. Fortunately, within half a day, I had also mobilized a number of young refugees from all parts of the camp. Using the information we had received from the medical team, we made a number of public health campaign posters. The next day, we put them up at several points in the camp. At the same time, each one of us had the duty of visiting people in the camp and sharing with our families and neighbours all the relevant information we had been given on Covid-19. These were the first tasks undertaken by our Corona Awareness Team, formed by a number of young residents of Ritsona.
When the number of infected people was first announced, everybody was scared. All offices and common spaces were closed down, but the large majority of the residents of the camp had little in the way of information – or, worse, had been exposed to harmful misinformation about the virus. The aid organizations, once active in the camp, kept their distance and avoided getting close to anyone. Gradually, panic spread among all residents, leading to a chaotic and explosive situation with fights among some of the infected residents. The medical personnel, feeling unsafe in their workspace, left the camp.
The situation became truly critical: we had no time to lose. We plucked up all our courage and took it upon ourselves to speak to the various communities, informing them about the measures they needed to take to protect themselves, their families and their neighbours. The first step we asked them to take was to stay as much as possible in their containers. At the same time, we organized competitions and activities that would highlight the epidemic, its effects on different age groups and the behaviours that would protect people from infection.
Realizing that more needed to be done, I decided to organize a refugee-led self-educational programme by soliciting the collaboration of other young refugee women who had had some teaching experience in their countries of origin. The programme started a few days later. It attracted lots of people, especially from the Syrian and Kurdish communities, who felt that their women and girls would be in a safe place, run by young women, with no men around. Our self-organized classrooms offered a good opportunity and an easy way for the Corona Awareness Team to disseminate concrete, accurate information for them to then share with the rest of the residents.
The team consisted of 17 young refugee girls who started an open and inclusive programme to enable residents to pursue some sustainable goals in the midst of the pandemic. Another objective behind this programme was to draw on the skills and abilities of girls, to help them access knowledge and develop confidence in themselves. We believed that this would contribute to a decrease in male violence and aggression toward women and girls.
Since then, the project has continued to evolve. As we have classes in the camp, there is still a programme of information-sharing between teachers and students, but we realized it was important to find sustainable ways to communicate to the wider community too. With this in mind, we launched a poster-making campaign, installing them in frames on walls and trees as a reminder. Another of our activities is having paintings in the containers: this is a good way to illustrate how to protect ourselves from Covid-19 while also giving some colour to the drab surroundings of the inhabitants of Ritsona.
In a camp, if you cannot find any opportunities to develop and enrich yourself, you need to make them. Similarly, if there is no suitable space available in which to act, you should create one and involve other people in doing so. And if you are not visible, you should put as much effort as you can into being seen, grabbing the attention of the world outside and attracting the lenses of cameras to where you live. Everyone has been affected by the pandemic – but everyone, too, has the possibility to take action to make themselves and their communities safer from its terrible effects.
Photo: A portrait of Parwana taken in Ritsona, Greece. Credit: Tom Alboth.
-
By Zita Holbourne
Newham, a deprived borough in East London with a high proportion of ethnic minority residents, has been one of the areas in the United Kingdom (UK) hardest hit by Covid-19. As a race equality and anti-austerity campaigner working for decades with local communities, I was not surprised by this.
After more than a decade of government austerity, with the deepest cuts being made to the poorest boroughs, the virus has exposed the profound shortfalls in health and well-being caused by discrimination. This has been the reality for many of Newham’s residents long before the latest crisis, reflected in the fact that on the eve of the pandemic it had the highest tuberculosis rates in the UK, at 47 cases per 100,000 people in 2018 (2.5 times the rate for London as a whole and 5.5 times the rate in England during the same year).
While Newham is notable for its diversity – some 71 per cent of Newham’s population is Black, Asian and minority ethnic, according to the 2011 Census – it is also one of the most deprived boroughs in London, with 37 per cent of its population living in poverty, second only to neighbouring Tower Hamlets in this respect. It is perhaps not surprising, given the area’s history of marginalization, that it soon became a major epicentre in the first weeks of Covid-19’s spread: by the beginning of May, Newham was reporting the highest death rate of any borough in the country, with 144.3 deaths per 100,000 people. Black, Asian and minority ethnic people live in the most deprived areas of the UK because of the institutional racism they face in every aspect of life, including housing, employment and services. We have heard politicians and pundits declaring that the virus does not discriminate, but the social conditions that have led to Black, Asian and minority ethnic people dying do, leaving our communities two to three times more likely to die of Covid-19 than the general population. In Newham, the interplay of a number of factors closely tied to discrimination and exclusion has been deadly and enduring — over the course of the first year of the pandemic, it registered the highest excess death rate in the country.
One significant issue for Newham community members is the discrimination many face in the labour market and in employment. As many as 36,000 residents do not receive the minimum wage, let alone a living wage sufficient to meet their basic needs in London. They are more likely to work in precarious jobs or in frontline roles as key workers in areas such as social care, public transport and food supply. Often without the option to work from home and lacking adequate personal protective equipment, they can face considerable potential hazards associated with their work — yet even those at high risk may feel unable to stop working in order to shield, protect loved ones or to recover when they contract the virus, because they cannot afford to do so.
By the beginning of May 2020, Newham was reporting the highest death rate of any borough in the country, with 144.3 deaths per 100,000 people.
Another critical factor is the prevalence of sub-standard housing and living conditions that enable the rapid spread of Covid-19. Newham has the worst overcrowding rates in the UK and is notorious for rogue landlords exploiting tenants desperate for accommodation. This had led to the scandal of people being housed in sheds and garages, as well as large numbers of migrant families squashed into small houses and flats — with sometimes three or four families living in a single two-bedroom property. In one notorious case in 2015, 26 people were found living in a three-bedroom property. In most instances, however, these abuses go unreported.
Newham has seen much ‘regeneration’ in recent years, yet this has not benefited the poorest in the borough, with insufficient affordable homes and social housing being built to offset the more expensive developments initiated during and after the 2012 Olympic Games in Stratford, a district in the north-western corner of the borough. As a result, many poor working-class families have been priced out of the area. This is the latest episode in a long process of displacement that stretches back to the era of Prime Minister Margaret Thatcher, when the introduction of the right-to-buy scheme meant that a lot of council housing became privately owned while no further social housing was built to replace it.
Nowadays, new-builds attract wealthier buyers to the borough. Prior to this, some high-rise council buildings had begun to be knocked down, but now developers build even taller apartment blocks, but for the luxury market. Meanwhile, the poorest residents in Newham have until recently continued to occupy hazardous, cheaply constructed housing. For example, a number of tower blocks in Newham were insulated with the same dangerously flammable material that was used on Grenfell Tower, where a fire broke out in 2017, leading to 72 people losing their lives. The Newham authorities have finally completed the removal of this sub-standard cladding from all council-run housing.
For the few residents who are still able to access social housing, usually as a result of an emergency or profound trauma, securing different accommodation as your circumstances change can be incredibly challenging. If, for example, you are a single person who then has a child, or a family with one child who then has two more, you will not be rehoused to a larger property and are told that you have to wait until your child is a teenager. This means that the only options you have are either to get a mortgage to buy a property yourself or to give up your social housing to rent on the private market.
For most, of course, neither is an option. Low pay, precarious work and zero-hours contracts — all issues impacting disproportionately on ethnic minorities — make securing a mortgage close to impossible, especially for young people with young families. Likewise, giving up the relative security of social housing to brave the private market, with its exploitative landlords and sub-standard housing conditions, is not something most would choose to risk. Anyhow, the huge cost of renting privately a property that meets your family needs makes it an unaffordable option. As a result, many have no choice but to continue to live in appalling conditions indefinitely. I have heard of families with five children forced to live in a two-bedroom property for several years.
I know this, too, because I have had to navigate this opaque and inhospitable system myself. The flat that I lived in when my baby was born years ago was in one of the Grenfell-style blocks, initially earmarked for demolition before the authorities instead renovated the building but applied the same dangerous cladding to it. As my son grew up, I tried every route possible in order to get a larger property than the one-bedroom flat we were living in. The council told me I would have to wait until my son was a teenager to be rehoused. I tried the council exchange system, but of course nobody wanted to give up their two- or three-bedroom property for my one-bedroom property — so it was impossible.
At the time, however, there was a scheme where you could receive a set amount of money as a down payment on your mortgage if you gave up your council property, and in the end this is what I was forced to do — but I was also fortunate to be able to do so because I had a secure full-time job. While this was a better alternative than exercising the right-to-buy, because at least it freed up the property for someone else who needed social housing, for the many Black, Asian and minority ethnic workers living in the borough who lack secure or adequately paid work, this is not an option.
And so the same cycle of bad housing, low pay and deprivation continues, impacting disproportionately on ethnic minority and migrant communities in London and elsewhere. This is why Covid-19 has exacted such a heavy toll in Newham. While the past year has been one of trauma and difficulty for everyone, for the most deprived communities the impacts have been devastating. While race equality activists have long highlighted that racism kills, the pandemic has brought this hard truth into plain sight, with a virus that appears to flourish alongside discrimination and exclusion.
Covid-19 would seem to offer clear proof that institutional racism can lead not only to reduced life chances but also to severe illness, disability and death. Yet in March 2021, a year on from the onset of the pandemic, the government published its Race Commission report — a document which was immediately met with shock and outrage by race equality campaigners, historians, health experts, researchers, academics and community members for suggesting that, in fact, institutional racism did not exist. This bodes ill for any hopes of a transformative, rights-based approach to public health through more equitable housing, employment and services. Until the reality of racism is recognized and addressed, minority ethnic communities in Newham and across the UK will continue to suffer from its effects.
Photo: Focus E15 Mothers Chain of Power protest the scandal of Newham Council leaving 400 empty homes at the Carpenters Estate while those living at the Brimstone House hostel and many others need safe housing, Stratford, Newham. Credit: JESS HURD/reportdigital.co.uk.
Environment and land
Promote land rights, environmental protection and access to green space to support resilience and recovery during the pandemic, as well as prevent future crises: While land grabbing and deforestation have increased around the globe, community-led conservation and engagement in the natural world have the potential to improve social and environmental well-being. The disruption of the pandemic and the restrictions imposed to contain it have enabled even greater impunity for armed groups and militias to attack indigenous and environmental defenders. At the same time, logging, mining and agricultural expansion have accelerated forest clearance across the world, in the process spreading Covid-19 into remote areas and risking the emergence of new zoonotic diseases in future. This has underlined the importance of securing community land rights for preserving fragile environments from degradation and destruction, particularly in indigenous territories. At the same time, the experience of lockdown and other restrictions has also underlined the importance of equitable access to parks, gardens and green space in towns and cities, especially for marginalized minorities.
- 01

Brazil: For the Amazon’s indigenous peoples, Covid-19 is the latest crisis in a long history of exclusion
By Genna Naccache Even before the outbreak of Covid-19, indigenous peoples in the Amazonian basin were confronting a crisis that has been decades in the making. Brazil’s development policies, based on widespread exploitation of the…
0 min read
- 02

Rwanda and Uganda: For Batwa communities, poor health outcomes are a symptom of protracted discrimination
By Hamimu Masudi In anticipation of a lockdown, when everyone was busy stockpiling all sorts of household items, a leader of an indigenous hunter-gatherer community in East Africa sent an email to his contact at Minority Rights Group…
1 min read
- 03

United Kingdom: Equitable access to nature is more important than ever since the pandemic
By Mya-Rose Craig In the first weeks after lockdown started in the United Kingdom (UK), reports began to emerge that Visible Minority Ethnic (VME) people were dying from Covid-19 in increased numbers. Yet at the time there was not…
1 min read
-
By Genna Naccache
Even before the outbreak of Covid-19, indigenous peoples in the Amazonian basin were confronting a crisis that has been decades in the making. Brazil’s development policies, based on widespread exploitation of the country’s non-renewable natural resources, including its rainforests, have long been a major cause of encroachment on indigenous peoples’ lands.
Indigenous territories are largely unprotected from the threat of industrial-scale extractive activities such as logging and mining, often imposed by public authorities without any consultation with local communities or respect for their land rights. The projects are frequently accompanied by systematic campaigns of intimidation and violence against indigenous peoples and environmental defenders, with dozens of activists killed or injured in recent years.
These depredations have only intensified since the election of the far-right politician Jair Bolsonaro as the country’s president in January 2019. Having explicitly vowed to roll back environmental protections and promote the development of the Amazon region, Bolsonaro has overseen a dramatic escalation in the assault on conservation areas and indigenous territories. Against a backdrop of increasing impunity, illegal clearance for logging and cattle farming rose sharply in the months after his election: data released by the National Institute for Space Research in August 2019 showed that forest fires in the Amazon had increased by 84 per cent compared to the same period the year before. This has been enabled in part by the government’s transfer of deforestation management responsibilities, previously under the aegis of the Environment Ministry, to the Agriculture Ministry — an institution that has repeatedly encouraged the clearance of rainforest to accommodate cattle farming, plantations and other infrastructure projects. Enabled by the government’s development policies and with global demand for exports such as soya for farm feed and sugarcane for biofuel on the rise, Brazil’s landscape has suffered irreparable damage.
This continued expansion deep into the Amazonian rainforest poses a grave threat to the region’s indigenous populations and its rich biodiversity. Furthermore, given the vital role of the Amazon’s forests in reducing greenhouse gases, absorbing carbon dioxide and regulating global climate patterns, Bolsonaro’s destructive policies have attracted alarmed responses from scientists and activists across the globe. The greatest concern is that the Amazonian ecosystem is fast approaching a point of no return, after which forest cover will give way to cerrado, a savannah-like state that no amount of human intervention will be able to restore. Some scientists predict that the region may be as little as 10 years away from reaching this tipping point: from then, it may not only stop absorbing CO2, but also contribute to its increase in the atmosphere.
Data released by the National Institute for Space Research in August 2019 showed that forest fires in the Amazon had increased by 84 per cent compared to the same period the year before.
Furthermore, the government’s plans to extend its road network deeper into the Amazon could escalate deforestation and environmental collapse. Road building in the Amazon is rooted in the military dictatorship, beginning with the inauguration of the Transamazonian Highway in 1972, passing through seven states and stretching over 4,000 kilometres. Its construction led to the clearance of vast areas, cutting through the territories of 29 indigenous peoples, of whom 11 had previously been isolated. The ‘pacification’ and removal of the indigenous inhabitants by force involved displacement, torture, massacres and the spread of diseases such as smallpox, both through negligence and intentionally. In the process, indigenous populations were decimated: for instance, an estimated two-thirds of Panará in Mato Grosso and Pará died during this period. This remains a painful reminder of the catastrophic human, cultural and ecological consequences of the military regime’s land expropriation and exploitation in the 1970s.
The Transamazonian Highway project was largely abandoned for over four decades. However, Bolsonaro has made its resumption a central policy of his administration, paving the way for further human settlement and exploitation of its fragile ecosystems. Not only will these new roads provide loggers and miners with greater capacity to transport their goods and expand their activities, but they will also open up access to land which could potentially be deforested and sold for agricultural purposes. Such projects are heavily underpinned by foreign and multinational capital interests. The growing demand in China for soya and beef, for example, has driven deforestation in the Amazon as vast swathes of land have been given over to industrial agriculture. Besides posing a major threat to endangered wildlife, medicinal plants and pristine river basins, these activities are also the main driver of indigenous land rights violations.
Other invasive developments are on the horizon, such as the industrial-scale Baron of Rio Branco project, which aims to develop the remote northern state of Pará in the Amazon, home to uncontacted indigenous communities. This project will involve the construction of a major hydroelectric dam, the Oriximiná, the construction of a bridge, and lastly, the extension of the busy BR-163 highway through hundreds of miles of protected indigenous forestland. Regrettably, this only confirms Bolsonaro’s determination to completely centralize control over the fragile Amazon basin.
These threats have been exacerbated by the onset of the pandemic. Paradoxically, reduced social contact and travel restrictions have played into the hands of loggers, miners and farmers, who have been able to escalate their illegal clearance of rainforest as the number of conservation officers and personnel monitoring violations in the field were reduced. In the first four months of 2020, during which millions of Brazilians opted to stay at home despite the mixed messaging of the Bolsonaro administration, deforestation in the Amazon rose sharply: an increase of 55 per cent in the first four months of 2020 compared to the already high levels seen in the same period of 2019. This trend continued throughout 2020, culminating in the highest annual level since 2008.
Brazil’s indigenous populations have a long history of devastating health crises, from measles to smallpox, brought into their communities from elsewhere. These outbreaks have often been closely linked with colonialism and land rights violations: during the 1980s, for instance, an influx of gold miners into Yanomami territory not only brought violence and destruction but also the introduction of a host of unfamiliar diseases that proved deadly for the community, killing around 20 per cent of its members in less than a decade. A similar pattern has emerged since the onset of Covid-19: the thousands of illegal miners and loggers active in the Amazon are widely believed to have contributed to the transmission of the virus, bringing it to even remote communities which might otherwise have been protected by distance and isolation from its spread.
The construction of the Transamazonian Highway passing through seven states and stretching over 4,000 kilometres cut through the territories of 29 indigenous peoples, of whom 11 had previously been isolated.
Indeed, throughout the pandemic, indigenous peoples in the region have been especially vulnerable, with evidence suggesting mortality rates among these communities are more than double the national average. This heightened susceptibility is due to a range of factors, including the limited availability of health care, the prevalence of other underlying conditions among the population and their lack of exposure to other commonly circulating diseases. There are particular concerns about the implications for the more than 100 uncontacted tribes living in the rainforest who could be decimated if the virus reaches them. Strikingly, indigenous activists and political opposition groups have explicitly framed the pandemic as a potential ‘genocide’, that is, not as an isolated crisis but part of the broader pattern of death and disease that has accompanied the encroachment on and exploitation of their lands. This perception has only been reinforced by the government’s apparent willingness to roll back protections in the midst of the pandemic: indeed, in May 2020 leaked video footage appeared to show the Environment Minister suggesting that the crisis offered an opportune moment to ‘run the cattle herd’ through the Amazon while the public was distracted.
Early in the pandemic, between January and April 2020, deforestation in the Amazon rose sharply: an increase of 55 per cent compared to the same period in 2019.
Indigenous peoples in the Amazon have also experienced great suffering and cultural attrition through the loss of their elders to Covid-19. As storehouses of ancestral knowledge and wisdom, as well as vital guides to everything from local languages to traditional medicines, their deaths have left a profound absence in the collective knowledge of their communities. Alongside their critical role as ‘living libraries’, they also served as leaders to resist the countless invasions of their land and to protect their forests at all costs. The decimation of the older generation has therefore dealt a heavy blow to the unique identities and traditions of their peoples.
While the Bolsonaro administration has repeatedly sought to minimize the threat of Covid-19, the virus has torn through much of the country, with the Amazon’s capital city, Manaus, known as the gateway to the rainforest, emerging as its epicentre. Images from the city of mass graves and harrowing accounts of patients dying outside hospitals, of families desperately scouring the city for oxygen cylinders to keep loved ones alive, have captured the government’s negligent response to the crisis. After a brutal wave in the first months of the pandemic that many hoped would spare its residents from another surge in infections, the beginning of 2021 saw the city enter another crisis amidst the emergence of a deadly new variant in the region. While the implications could extend well beyond the Amazon and even Brazil – the variant has since spread to dozens of countries and prompted one renowned epidemiologist to warn that the government’s failure to manage the virus could turn the country into a threat to global health as a ‘breeding ground’ for further mutations – it seems inevitable that the heaviest burden, yet again, will be borne by indigenous peoples themselves.
Photo: From their villages on the banks of the Branco River in the Amazon, members of the indigenous Matis community travel for 12 days to Atalaia do Norte, the town closest to them, to get vaccinated against Covid-19. Credit: EPA-EFE/Tatiana Nevo.
-
By Hamimu Masudi
In anticipation of a lockdown, when everyone was busy stockpiling all sorts of household items, a leader of an indigenous hunter-gatherer community in East Africa sent an email to his contact at Minority Rights Group International (MRG). It was a photo of a plant, traditionally used in bathing, that produces lather when crushed in water. He wanted to learn from her if this plant would be suitable for handwashing, as a precautionary measure against Covid-19.
His contact reached out to a specialist chemist who responded after a short while. ‘Any plant that produces lather will be effective’, the chemist replied. ‘And under circumstances where a family must choose between spending on food and spending on soap, they should choose food to help protect the immune system and use the readily available plant in washing.’ The advice was well received and was shared widely within indigenous peoples’ networks in the region.
In a world engulfed by the pandemic, this is just one snapshot of the unique struggles that indigenous peoples in Central Africa face. With a long history of devastation and dispossession, Batwa, Mbuti and Baka communities were fighting for their survival long before the advent of Covid-19. Forced off their land and prohibited from entering much of their former territories to gather food, firewood or medicinal herbs, their situation has become even more precarious since the arrival of the virus. Alongside adults with underlying health conditions and older people, indigenous people are known to be at higher risk from emerging infectious diseases.
Even though these communities consistently face poorer health, including mental health outcomes, exacerbated by the stigma and discrimination they face, they remain outside formal social protection systems and are unable to access medical and financial support. For instance, Batwa in Rwanda and Uganda were reportedly left out of the national emergency food distribution and have been dependent on the goodwill of members of other better-off communities and local charity organizations. A rapid phone call survey of Batwa communities by activists in Rwanda, a fortnight into lockdown, revealed a lack of appropriate information on public health and impractical official hygiene requirements ill-suited to the local context.
Drastically reduced numbers of visitors because of the impact of the pandemic on the tourism sector has devastated local livelihoods. By selling handicrafts, pottery and tour-guide services, indigenous communities were able to earn incomes and sustain their livelihoods – but these opportunities have been significantly depleted by Covid-19 containment measures. Farming, which would once have offered an alternative source of income, is not an option for most due to the systematic dispossession of indigenous peoples from their lands, beginning in the nineteenth century under European colonial rule and continued by successive post-colonial African states.
As pandemics tend to deepen existing inequalities, the risks are especially high for indigenous women. According to traditional norms, they are the default caretakers of children, the sick, the elderly and members of their extended families. The risks of abuse and exploitation are readily apparent, particularly in the context of a major health crisis, and reports of gender-based violence have been documented by non-governmental organizations working with Batwa communities in south-eastern Uganda, for instance.
Across Central Africa, the tragedy of indigenous peoples lies in their invisibility, as many laws in these countries remain silent as to their existence – a factor that explains the limited availability of disaggregated data on infections and other epidemiological data. This is also reflected in the absence of public health information specifically targeted at indigenous peoples and their lack of representation on national Covid-19 task forces. This is despite recommendations by the United Nations ‘to ensure these services and facilities are provided in indigenous languages, and as appropriate to the specific situation’ of communities.
The plight of forest peoples in Rwanda, Uganda and other countries across Central Africa not only illustrates the need for tailored, accessible and culturally appropriate interventions in the midst of a pandemic. It also reflects how the legacy of landlessness and dispossession has affected every aspect of their lives, from health and livelihoods to participation and well-being, long before the pandemic began.
Photo: Baleku Flora (centre) was born in the forest and left with her parents when the government started conserving the forest for Mountain Gorillas. She later went back to live on the outskirts of the forest with her husband who died before the government forced every Mutwa out of the forest in 1991. With her family, she now lives in Buhoma, a village bordering the Bwindi National Park. Credit: Esther Ruth Mbabazi.
-
By Mya-Rose Craig
In the first weeks after lockdown started in the United Kingdom (UK), reports began to emerge that Visible Minority Ethnic (VME) people were dying from Covid-19 in increased numbers. Yet at the time there was not sufficient public data available for the government to determine how many exactly: while information about the ethnicity of the deceased was being collected by health care providers, this did not appear on death certificates. So, while it was possible to calculate the percentage of those dying in hospitals and care homes who were VME, this data was not being formally collected or made publicly available.
Nevertheless, it was evident that VME people were being disproportionately affected: a study published in early April 2020 found that, despite making up 14 per cent of the population in England and Wales, 35 per cent of almost 2,000 people in intensive care at that time were VME. This disparity was not only visible among patients but also among health workers who themselves became infected: all of the first 10 National Health Service (NHS) doctors to die from Covid-19 were VME. While VME NHS staff were contracting and dying from the virus in greater numbers, they also had to contend with the effects of structural racism in their workplace – the impact of bullying and harassment, longer and more dangerous shifts, personal protective equipment (PPE) shortages, isolation and lack of translated information on how to avoid contracting Covid-19.
By the third lockdown, we knew that people of Bangladeshi and Pakistani ethnicity, like my family, were twice as likely to die of Covid-19 compared to a white person. With 30 per cent of UK Bangladeshi families living in overcrowded conditions, this was not so surprising. Many non-NHS frontline workers were also VME, such as bus drivers, taxi drivers, take-away staff, shopkeepers, supermarket staff and care workers.
It has been well known for many years that VME communities are affected by mental health issues at much higher rates and are far more likely to be diagnosed with a mental health illness, including serious conditions such as schizophrenia or bipolar disorder. Of those admitted into mental health wards, a significant proportion are VME. The reasons are thought to be poverty, overcrowding, racism, mental health stigma and other factors associated with inequality. However, I believe that one reason not considered by white researchers is the lack of access to green spaces, which is known to be essential for helping anxiety, depression and well-being.
Most VME communities live in the centre of our towns and cities, where the green spaces are degraded and parents have concerns about their teenagers going out alone, due to worries such as their children being labelled as troublemakers by the police or getting involved in drug running. During the pandemic, VME people talked about their narrow roads being blocked by neighbours working from home and parking on pavements, making it harder for people to move out of each other’s way.
Of those admitted into mental health wards, 60 per cent are Visible Minority Ethnic. The reasons are thought to be poverty, overcrowding, racism, mental health stigma and other factors associated with inequality.
I have been birding all my life and have always understood how being outside in nature helps my mental health. When I was 13 years old, I organized my first birding camp for VME teenagers from inner-city Bristol, who loved being in the countryside. Until then, I had thought my British-Bangladeshi cousins did not want to go into nature because they thought it was boring, rather than because they had never had the opportunity and never had it made relevant to them. Many events later, I have had a 100 per cent success rate in getting VME children and young people engaged with nature. The work of Black2Nature, the charity I set up soon afterwards, has become even more important during lockdown. This is why we have organized numerous activities and tree-planting days for VME families and young people: getting VME people out into the countryside and getting them engaged with nature has been essential for their mental health.
Black2Nature has had to change the way we run our camps due to Covid-19. As we have been unable to run overnight camps, we ran VME family nature days in August 2020. Family bubbles joined us for nature activities including bird ringing, nature walks and pond dipping. The children, parents and grandparents learnt a lot about nature and wildlife. They were able to see birds up close during the bird ringing, and some even released them from their hands afterwards. The nature walks included bird watching from the local hides. Black2Nature helped the families, especially the children, to identify some of the different bird species. The pond dipping allowed the children to look at minibeasts up close and, using identification cards, they were able to work out what each creature was.
The families who came to our nature days had been particularly struggling during the Covid-19 pandemic. One Pakistani family who attended had been hit financially. The father was a taxi driver and the sole earner for the family. His employment had been directly affected by the pandemic, causing him to lose the family income. None of the families that joined us had had opportunities to engage with nature in this way before. The families were also treated to halal fish and chips and ice-creams. With family incomes reduced to social assistance, the mums told us that this was their treat of the summer, their summer holiday. Another Bangladeshi family who attended had an autistic teenage son with high support needs. They had felt trapped, unwelcome and unable to go anywhere without being judged and feeling ill at ease. On the nature walk, they were able to go at their son’s speed so that he was able to learn and participate as well.
Black2Nature ran two tree-planting days in December 2020 and four more days in March 2021 at the Strode Valley Land Project. We planted 1,000 trees, some of which were marked by ribbons so that returning volunteers could identify them.
Black2Nature ran two tree-planting days in December 2020 and four more days in March 2021 at the Strode Valley Land Project. We had more than 250 people attend, with both lunch and transport provided. The majority of our tree-planting volunteers were from VME communities, many of them in groups of three generations who had come together to plant a tree for a family member who had passed away from Covid-19. We also had VME home-schooling families who struggled to find free activities to take part in. The children were eager to learn about nature and the benefits of trees.
We planted 1,000 trees, some of which were marked by ribbons so that returning volunteers could identify them. We are organizing tree-care days for the summer so people can return and help with the aftercare of the trees, and also to remember their loved ones. The impact of the pandemic and lockdown has been huge on everyone, but especially on VME people, often trapped inside high-rise flats. Getting outside and engaging with nature is so important, especially for supporting all our mental health and well-being.
Photo: A portrait of Mya-Rose Craig.
Livelihoods
Ensure that decent work, labour rights and adequate welfare assistance are a central part of any public health strategy, protecting those whose livelihoods are most at risk: Minorities, indigenous peoples and migrants, working disproportionately in precarious or informal employment, have been among those worst affected by poverty, food insecurity and evictions as a result of job loss or reduced income. While lockdowns, restrictions on movement and other measures have sometimes been necessary to contain the spread of Covid-19, their economic fallout has proved devastating to communities already contending with social exclusion. For many of those on daily wages, zero-hour contracts or working as waste pickers, street vendors or in other informal occupations, there has been little or no assistance from either governments or employers to help them weather the crisis. Indeed, in some cases even the limited rights in place before the pandemic have been rolled back, particularly for migrant workers and foreign labourers, who have experienced a rise in arbitrary dismissal and exploitation. The pandemic has therefore again highlighted the urgent necessity of social assistance and protections for all workers, regardless of their sector or migration status – and the cost to public health, through hunger, homelessness and other impacts, when these are not in place.
- 01

Afghanistan: ‘I had to ignore the threat of Covid-19 because I had to pay back my loans’
By Ali Amani and Ali Shaheer Afghanistan’s Sikh and Hindu communities have a long history in the country, with more than 200,000 living there until the 1990s. Since then, their numbers have steadily dwindled as conflict and discrimination…
0 min read
- 02

Bangladesh: Indigenous workers face unemployment and destitution in the wake of the pandemic
By Sanjeeb Drong It is widely recognized that indigenous peoples are among the most vulnerable and marginalized communities in Bangladesh. Historically, the country’s indigenous population has faced systematic discrimination,…
1 min read
- 03

Canada: Essential, but unprotected – Toronto’s racialized labour force
By Miriam Puttick In March 2020, as the World Health Organization declared the outbreak of Covid-19 a global pandemic, a sense of shared vulnerability dominated public discourse in many jurisdictions – the idea that the virus affects…
1 min read
- 04

Serbia: With livelihoods devastated by the pandemic, Roma struggle to make a living
By Boris Sijerkovic, Praxis At the entrance to an informal Roma settlement on the outskirts of Belgrade, there is a water tank. The settlement has no communal infrastructure and entire families live in small improvised houses of just a few…
1 min read
-
By Ali Amani and Ali Shaheer
Afghanistan’s Sikh and Hindu communities have a long history in the country, with more than 200,000 living there until the 1990s. Since then, their numbers have steadily dwindled as conflict and discrimination have forced many to emigrate. Today, only a few hundreds remain.
For this group, the pandemic has brought new challenges that intersect with other problems, including a spate of violent attacks by extremists. For the significant number of community members engaged in herbal medicines, however, the situation has also seriously affected their livelihoods, placing further pressure on them.
Sher Singh, 57, borrowed 100,000 AFN (US $1,300) from a local bank a year ago to expand his small herbal and Unani medicine shop. With the income he had from his shop, he had predicted that by paying 10,000 AFN each month, he would be able to repay the bank loan in the next 10 months and also make ends meet for himself and his family. But there was one thing that, like everyone else, he had failed to take into account – the outbreak of Covid-19 and its devastating impact on public health and the economy.
Twelve months after receiving the loan, Singh has only been able to repay 10,000 AFN – and on top of this the bank has issued a fine for late payment. While he earned as much as 24,000 AFN a month before the pandemic, with the spread of the virus and the subsequent lockdowns across Afghanistan, his income has halved. ‘I had never imagined that coronavirus would have such a negative impact on our livelihoods’, he says. ‘I took the loan thinking that my income would be 20,000 AFN, the same as the previous year, out of which I would spend 10,000 AFN on household expenses and rent, and pay back the remaining 10,000 AFN to the bank.’
Singh’s shop is located next to the historic Gurdwara in Shor Bazar, the site of a brutal attack by ISIS in March 2020 that left at least 25 worshippers dead. While most of his relatives fled Afghanistan shortly after due to security threats, he was unable to do so because he had to repay the loan. Despite this uncertainty and weeks of lockdown, he did not lose hope in his business: he reopened his shop once restrictions were lifted, and was confident that he could pay off the bank loan. However, another disaster befell him and his shop on the morning of 6 February 2021, when a bomb exploded in his shop, destroying his herbal products and property. Sher Singh and his cousin were severely injured in the incident. Now he says he wished he had left Kabul like his other relatives after the ISIS attack: he has no idea how he can rebuild his business or repay his loan.
Gul Charan Singh, 25, also belongs to the Sikh minority and owns a herbal and Unani medicine shop in the eastern city of Jalalabad. He lives with his parents and three sisters, and is the sole breadwinner for the entire family. Although he does not have to pay rent for his shop, as it belongs to the Sikh Dharamsala, the outbreak of Covid-19 in Afghanistan has made it difficult for him to earn a living. Charan’s daily income is now less than half what it was before the pandemic. ‘I used to have a good income’, he says. ‘I could easily spend money on the household and other needs – sometimes I even sent money to my relatives abroad – but now I can’t even make ends meet for my own family.’
A number of other community members who make their living from herbal medicine report that, in addition to the lockdowns and a decline in customers, another difficulty is the closure of transportation and trade routes with neighbouring countries, including India, Pakistan and Iran. Prior to the pandemic, they were freely importing and exporting herbal and Ayurvedic products and medicines: this was an important source of income for them and without it many businesses are now struggling. At the same time, domestic demand has diminished as many customers are struggling to afford food, clothing and other basic needs.
While Afghanistan has witnessed a decline in infections in recent months, new cases of Covid-19 are still being reported and in the meantime the country is having to deal with the economic fallout. For millions of civilians, the immediate financial prospects are bleak. For marginalized communities such as Sikhs and Hindus, on the other hand, these pressures intersect with discrimination and persecution – issues that, without concerted efforts from government and society, could continue long after the pandemic is over.
Photo: An Sikh Afghan man accepts money from a customer at his traditional herb shop in Kabul, Afghanistan June 19, 2016. Credit: REUTERS/Mohammad Ismail.
-
By Sanjeeb Drong
It is widely recognized that indigenous peoples are among the most vulnerable and marginalized communities in Bangladesh. Historically, the country’s indigenous population has faced systematic discrimination, injustices and gross human rights violations, from destruction of forests and land grabbing to forced assimilation and educational exclusion. Decades of state-sponsored population transfers have also led to indigenous peoples becoming minorities in their own territories. Some indigenous communities even face the terrible threat of extinction. The government’s International Mother Language Institute conducted an ethno-linguistic survey and published a report in 2019. This survey found 41 mother tongues in Bangladesh, of which 39 are spoken by indigenous communities – and 14 of those are at risk of disappearing.
It is unsurprising, then, that Covid-19 has impacted the lives and livelihoods of indigenous peoples with particular severity. An indigenous non-governmental organization (NGO), Indigenous Peoples Development Services (IPDS), conducted a survey in June 2020 among indigenous peoples in the plainlands, spanning 28 districts, 1,205 families and 35 different indigenous communities. The results showed that some 92 per cent of community members had experienced a sharp loss of income due to the pandemic. As a result, the number of plainlands indigenous people living in extreme poverty had increased by 62 per cent since the beginning of the crisis.
A major cause of this sharp drop in living standards is the precarious nature of the employment in which Bangladesh’s indigenous peoples are generally engaged. Of respondents to the survey who had previously been in paid employment, 72 per cent had as a result of the crisis either been immediately laid off or furloughed, which, in the context of Bangladesh, means discharged from their duties with little or no compensation except for a promise of reinstatement at some future date. On top of this, access to emergency assistance among plainlands indigenous peoples is extremely limited. Over 60 per cent of respondents reported having received no relief whatsoever from either the government or NGOs since the beginning of the pandemic.
According to a survey in June 2020 among indigenous peoples in the plainlands, some 92 per cent of community members experienced a sharp loss of income due to the Covid-19 pandemic.
The issue of job precarity is especially acute in the garment sector, beauty parlours and domestic service, which are fields where large numbers of indigenous women and girls are employed in Bangladesh. The lack of employment protection and benefits in these sectors has meant that the country’s indigenous peoples have been highly vulnerable to a sudden and complete cessation of income as the economic impacts of the pandemic began to be felt. The gendered impacts of the crisis have been especially wide ranging, with female respondents reporting increased threats of rape and harassment, additional domestic labour and limited access to sexual and reproductive health services.
The impact on employment has had further knock-on effects for indigenous peoples living in urban rented accommodation. The sudden cessation of income has meant that they are having to take on debt in the form of deferred rental payments, forcing many into arrears. As a result, some are considering returning to their home villages. Their plight has been worsened by the fact that, in many cases, landlords have prevented them from leaving for their villages until rents are settled. This has led to distress sales of land and other assets by rural kinship groups to repay rent. The scale of this problem has been impossible to gauge.
Other key issues raised by the study include increased reports of racism and violence, inequitable distribution of humanitarian supplies and an increase in overt racism. For example, indigenous peoples with Tibeto-Burmese features report ‘corona’ as a new racial slur. Dedicated efforts by the government to address the particular problems of social, economic and political exclusion faced by indigenous peoples in general have been very limited. While a ‘Development Assistance for Special Areas’ fund exists under the Prime Minister’s Office specifically for this purpose, its efforts are inadequate and poorly targeted. This speaks both to the specific issue of the pandemic and its secondary impacts, as well as the more general problem of the lack of recognition of indigenous peoples in Bangladesh. With thousands of indigenous migrant workers involved in informal sectors such as domestic work and garment manufacturing, the limited financial assistance for low-income and precarious workers must be significantly increased, with more effective targeting of indigenous peoples in remote areas in particular, if they and their families are to survive this difficult time.
Photo: Indigenous women harvest paddy in Chittagong Hill Tracks in Bangladesh. Eleven indigenous communities live in the hilly lands and are dependent on Jhum crops. Jhum is the main crop for the tribal communities living in the area. Credit: Rehman Asad / Alamy Stock Photo.
-
By Miriam Puttick
In March 2020, as the World Health Organization declared the outbreak of Covid-19 a global pandemic, a sense of shared vulnerability dominated public discourse in many jurisdictions – the idea that the virus affects everyone, everywhere. But the subsequent course of the pandemic has shown that, far from affecting everyone equally, the virus has interacted with existing socio-economic disparities to create significantly worse outcomes for groups marginalized at the intersections of race, class and gender. As these inequalities have sharpened, the policy rhetoric of being ‘all in this together’ has rung increasingly hollow.
While public health measures such as physical distancing and remote working arrangements have protected employees whose jobs can be performed from home, frontline workers have continued to provide essential services to others during periods of lockdown, exposing themselves to heightened risks in the process. Given that many urban workforces rely heavily on immigrant, racialized and gendered labour to perform essential roles, it is no surprise that these groups have experienced worse health outcomes during the pandemic. While such racial disparities have been identified in many pandemic-affected cities, Toronto, Canada provides a particularly illustrative case study.
Toronto is Canada’s largest metropolitan area, an economic powerhouse, and one of the most diverse cities in North America – with 52 per cent of the population belonging to a racialized group. Like many other well-connected urban hubs, it quickly became an epicentre of infection when the Covid-19 pandemic hit the country. Yet, as community advocates struggled to respond to the needs of the most vulnerable, the absence of racially disaggregated public health data made it impossible to verify what many suspected – that the pandemic was taking a disproportionate toll on racialized workers.
Three months after the first Covid-19 case was detected in Toronto, the city’s public health authorities finally began to collect case data on ethno-racial identity (unlike the US, Canada does not systematically disaggregate public health data according to ethnicity). When the first dataset was released to the public in July 2020, the findings were striking. No less than 83 per cent of reported Covid-19 cases were among racialized groups, despite the fact that the latter accounted for just over half of the city’s population. Some groups included in the data – particularly those identifying as Arab, Middle Eastern, West Asian, Latin American, South East Asian and Black – were particularly over-represented. For example, Black people made up 21 per cent of reported cases but only 9 per cent of the population.
No less than 83 per cent of reported Covid-19 cases were among racialized groups, despite the fact that the latter accounted for just over half of the city’s population.
At the same time, mapping exercises showing the concentration of Covid-19 cases across Toronto’s neighbourhoods revealed that the city’s most racially diverse neighbourhoods had infection rates three times higher than the least diverse neighbourhoods. Covid-19 cases in these neighbourhoods were also more likely to lead to severe health outcomes, with hospitalization and ICU (intensive care unit) admission rates four times higher and death rates twice as high.
Why these discrepancies? The neighbourhoods with the highest infection rates are predominantly home to low-income, racialized workers, who are more likely to be classified as ‘essential’ and therefore continue working on the frontlines during periods of lockdown. They include delivery drivers, cleaners, cashiers, long-term care and personal support workers, taxi drivers and employees in retail, food service, manufacturing and transportation. These workers have kept core economic activity going, while also responding to increased demand for some services from wealthier workers staying at home.
The nature of many of these industries exposes workers to a higher risk of virus transmission. Many of these occupations cannot be performed from home and require employees to work in close proximity to others. For example, many large outbreaks in Canada and the US have been linked to meat-processing facilities, where employees on the production line work close together and the fast pace of work makes it difficult to adhere to mask-wearing and disinfection protocols. In Canada, 41 per cent of meat-processing workers are members of racialized groups. Work in the personal support and health care sectors also means an increased risk of exposure to disease and infection. Many of these occupations are highly feminized, meaning that immigrant and racialized women are often disproportionately represented. For example, in Toronto and other metropolitan areas, over 70 per cent of nursing, residential care and home care positions are filled by immigrants, most of whom are women.
While the nature of the job puts essential workers at risk, so does the structure of the employment relationship. Since the 2008–9 financial crisis, Toronto has become increasingly reliant on precarious labour, which has especially affected racialized, young and female essential workers. Precarious labour often means low-paying, part-time or temporary work without job security or benefits. The lack of paid sick leave in particular, as well as the presence of employer policies such as attendance bonuses, may incentivize employees to continue working while sick. Precariously employed workers often work more than one job to make ends meet, increasing their degree of contact with others, and are also more likely to have experienced reductions in their hours and overall income as a result of the pandemic. Racialized youth have been hit particularly hard by these developments. As of August 2020, the unemployment rate among racialized youth in Canada was 32.3 per cent, compared to 18 per cent for white youth.
In Toronto and other metropolitan areas, over 70 per cent of nursing, residential care and home care positions are filled by immigrants, most of whom are women.
The risks that racialized workers face on the job are compounded by factors outside the workplace. Low-income essential workers are more likely to rely on public transportation to get to and from work, putting them in close contact with others. This is particularly true for racialized women: according to the 2016 Census, 51 per cent of racialized women in Toronto relied on public transit for their commute, compared to 27 per cent of white men. The housing crisis in Toronto also means that low-income workers often reside in multi-member households, making it impossible to self-isolate at home. They are more likely to live in high-rise buildings in densely populated neighbourhoods, with limited access to outdoor space for physical activity. Women and girls from low-income households also have fewer supports to rely on when it comes to domestic work and childcare. They often shoulder a large share of those responsibilities themselves, making it harder to look after their own physical and mental health.
In the presence of structural inequalities such as these, the imposition of uniform public health policies leads to differential health outcomes for marginalized groups. Consequently, when lockdowns occurred in Toronto, high-income, predominantly white neighbourhoods saw rapid declines in the number of new infections, while the opposite happened in low-income, racialized neighbourhoods. This is consistent with decades of research on the close connection between health outcomes and socio-economic variables, including factors such as racial identity, gender and class. The Canadian Medical Association states that these ‘social determinants of health’ have a greater impact on individual and population health than biological and environmental conditions, and that their impact can even be greater than that of the health care system itself.
The experience of Toronto has highlighted the need for disaggregated data collection to inform an equity approach to public health and avoid the imposition of blind policies that do not account for racial and other disparities. There is already evidence of these policy failures being repeated, with early stages of the vaccine rollout criticized for bypassing the city’s racialized, working class neighbourhoods. Moreover, despite the clearly identified patterns in Toronto, public health authorities in Canada are still not collecting racially disaggregated case data at the provincial or national level. By overlooking the needs of those most vulnerable to infection, such policy choices not only harm marginalized communities, but also hold back societies as a whole from recovering holistically from the pandemic.
Photo: An employee walks past cordoned off aisles of non-essential goods at a Walmart store, as new measures are imposed on big box stores due to the Covid-19 pandemic, in Toronto, Ontario, Canada. Credit: REUTERS/Carlos Osorio.
-
By Boris Sijerkovic, Praxis
At the entrance to an informal Roma settlement on the outskirts of Belgrade, there is a water tank. The settlement has no communal infrastructure and entire families live in small improvised houses of just a few square metres, made of various materials such as wood panels and pieces of plastic sheeting. Only occasionally some walls are made out of solid construction materials. Nylon, wrapped as makeshift insulation over the low roofs, flaps in the wind. A pack of dogs follow people down the muddy path through the settlement to the place where two brothers, Kristijan and Dusan, repair the trailers they use to collect recyclable materials.
Their vehicles often break down and are not suitable for going to areas far away from their settlement. At best, they can earn €5 a day – which, minus the cost of petrol, leaves very little to live on. Their income has become more constrained since the pandemic, when the purchase price of the materials they collect fell sharply. During the first weeks of the crisis, when a curfew was in place, they had only a limited time to collect the few materials that were available: those caught outside by police during the curfew were reportedly heavily fined.
As Kristijan and Dusan do not have permanent residence registered they do not possess identity documents – and without these they are excluded from social services. Registration of permanent residence at the address of a social welfare centre does not work in practice due to earlier situations when various bills arrived at the address of the centre in this Belgrade municipality and no one collected them. Roma in this settlement do not have any other legal basis to register permanent residence and obtain documents, so they are left unable to access their rights.
Furthermore, in settlements such as this, without electricity, water and sewerage, it is difficult to live hygienically and adhere to recommendations related to the prevention of infectious diseases. The situation during the pandemic was further aggravated when 120 Roma health mediators across Serbia stopped working. And even though there is an ongoing vaccination campaign, the brothers cannot get vaccinated themselves due to their lack of documentation, since the state does not have mechanisms to keep vaccination records for undocumented people.
The pandemic was accompanied by an economic crisis that left Roma in the settlement especially affected. ‘We were literally starving,’ says Dusan, summing up the difficulties he and other waste collectors faced during the year. Not only did they not receive any form of public assistance during the state of emergency declared at the beginning of the crisis, but they were also left without the €100 of financial support given by the authorities to adult Serbian citizens in 2020, as applying for this type of assistance required possession of a citizen’s unique personal number (JMBG) and an ID card. Similar financial assistance announced for this year, amounting to €60 in total, given in two instalments, will not be accessible to them either because of the same documentation requirements.
The pandemic has also greatly affected Roma musicians living in settlements near Vladičin Han, a poor municipality in southern Serbia. The music industry as a whole was seriously disrupted and popular festivals cancelled, including the famous Guča Trumpet Festival. According to some estimates, around 7,000 musicians in Serbia were left without work, while the limited financial relief allocated from the budget was given to a few registered performers. After the end of the state of emergency, various measures were put in place to prevent the spread of the virus, leaving musicians with limited opportunities to make an income. Although cafés, bars and restaurants are currently allowed to operate if they have outdoor seating, live music in their facilities is not allowed. Roma musicians from Vladičin Han, who make a living through performances at celebrations, have not been able to do so for over a year now. As a result of the pandemic, around 600 of them, mainly unregistered trumpet players, have been deprived of their only source of income.
In the village of Prekodolce, famous for its trumpet players, the musicians proudly state that world hits such as ‘Mesecina’ and ‘Kalasnjikov’ were created in this very village. However, everything else they have to say refers to the problems that have multiplied and become even more visible in the past year. Twenty orchestras from this village have not performed since the outbreak of the epidemic. The work has stopped, but not the bills, which continue to arrive at their addresses.
‘I was wearing one mask for months, and it gives you protection for two hours, but I did not have the money to buy a new one,’ says Ahmed. ‘Many people were infected here, many of them died. The only assistance we received was from a local Roma organization: hygienic items, food, firewood. Before the elections, the Red Cross distributed some help, oil and flour.’
There has been little improvement for these musicians since the end of the state of emergency. Residents have tried to apply for support at the social welfare centre, but they were not recognized as persons in need and most requests were rejected out of hand without being reviewed in writing. Members of their orchestra have applied for numerous jobs since the outbreak of the pandemic, with local businesses and building companies, and seasonal work, but none of them were invited for interview, let alone employed. In the meantime music, their main source of livelihood before the pandemic, remains out of bounds.
Aleksandar brings out a dusty case which has not been opened for a year. A tenor horn is inside, an instrument he was given as a part of the readmission assistance provided to returnees when he came back from Germany. This instrument fed his family. Valves have tarnished as they have not been used, refusing to move when Aleksandar touches them. ‘It should be soaked in warm water for at least two or three days,’ Ahmed advises, ‘not now, but when necessary. If we could play, we wouldn’t request social assistance. Public enforcement officers came, they record your possessions even if you are not there. They recorded someone else’s concrete mixer which they found in my yard.’
‘We are loud, that is why we don’t work,’ concludes Dragan, one of the trumpet players. ‘Someone would report us to the police for violating the prescribed measures. Owners of the restaurant won’t have us either: “You are noisy”, they say. There are nine people in our orchestra – it is too many. We cannot play quietly and earn a living if we play somewhere for a few guests. We need celebrations where 200 people gather.’
The situation in Lepenica is even worse: more than 150 musicians here have been without work for over a year. They have been trying to find some engagements online, but without success. As no one contacted them, they went to Niš, Kraljevo and other regional centres on their own, hoping to be able to play and make some money. They were rejected everywhere, and even tried their luck in small towns where they faced warnings that they would be reported to the police if someone heard them play. ‘We only spent the money we don’t have on petrol,’ says Stefan, adding that he has been trying to find work, but only physically strong and skilled workers could be employed in the construction industry. ‘They wouldn’t even hire me to do scaffolding work.’
As they are not recognized to be in a state of need, unregistered musicians mainly do not exercise the right to access social assistance. State welfare centres have discretionary powers in determining who is eligible for support. Even when they do approve assistance, they can reduce it to account for so-called ‘missed earnings’, which is the amount the beneficiary could have earned if they so wished. However, the centres are not obliged to prove that work opportunities were available. This means that arbitrary decision-making largely goes unchecked.
Of all the families in Lepenica who earned their living through music, only one or two are still able to pay their bills. Electricity and water connections have been switched off for most households. When they were left without water, they did not even have use of the municipal sewerage system. As a result of these inhumane conditions, the residents of this settlement were forced to connect illegally to water and power supply systems on their own. The employees of utility companies would then come again and take the water meters and switch off the electricity meters. Enforcement officers came to their settlement as well but there were no items of value to record or take away with them. Without electricity and internet access, most children from this settlement were not able to engage in online learning. Knowing their hardships, shopkeepers in Lepenica let many residents purchase groceries on credit, trusting that they would pay once they are able.
Trumpet players face an added stigma due to the risk associated with their instrument and its apparent ability to spread aerosols several metres. Their only hope is that eventually, once infections reduce and restrictions begin to relax, a negative PCR test or a vaccination certificate may allow them to resume work. Until then, there is an urgent need for comprehensive social assistance and additional targeted support for those worst hit by the pandemic, regardless of their registration status, to reduce the suffering brought on by the crisis and prevent further worsening inequality for the country’s most marginalized communities.
Photo: A Roma music band composed of trumpet players perform in the streets of Belgrade, Serbia. Credit: Jerome Cid/Alamy.
Language and education
Educational initiatives must ensure that all students, including those from minority and indigenous backgrounds, are adequately supported: Lack of computers and other equipment, compounded by language barriers, have widened inequalities and also limited access to essential public health information. Education has been a prominent casualty of the pandemic, as students have had to adapt rapidly to school closures and the transfer to online classes. For children belonging to minority and indigenous communities, many of whom already faced multiple barriers in accessing education, these difficulties have only intensified – particularly for those with little or no access to a computer or internet connection. The effects are likely to be especially acute in the learning of minority and indigenous languages, an area that has long been poorly prioritized in many countries. Yet the pandemic has also illustrated the vital importance of multilingual resources. With public information campaigns frequently failing to engage non-majority populations, community activists have mobilized to communicate life-saving guidance to others in their native languages.
- 01

Algeria: The ongoing struggle of indigenous Tamazight speakers in the wake of the pandemic
By Silvia Quattrini When Covid-19 hit Algeria, the country was entering its second year of peaceful protests, globally known as the Hirak (Arabic for ‘movement’). Protesters first took to the streets in February 2019 calling for the removal…
0 min read
- 02

Ukraine: Local Roma initiatives to tackle educational inequalities during the pandemic
By Yulian Kondur and Nina Henke Besides its devastating health impacts, Covid-19 has further marginalized whole communities and is exposing long-standing inequalities. This is especially evident in the area of education. Distance and online…
1 min read
-
By Silvia Quattrini
When Covid-19 hit Algeria, the country was entering its second year of peaceful protests, globally known as the Hirak (Arabic for ‘movement’). Protesters first took to the streets in February 2019 calling for the removal of President Abdelaziz Bouteflika, who at the time was seeking a fifth term in office after two decades in power.
Although Bouteflika was removed in April 2019 by the army, the movement continued to push for a more fundamental transformation of the corrupt political system.
The controversial election of Abdelmadjid Tebboune in December 2019, a former prime minister under Bouteflika, did not meet the movement’s expectations. However, when in March 2020 the Algerian government announced a series of restrictive measures in response to the first registered death from Covid-19 in the country, the Hirak also decided to suspend their weekly Friday and Tuesday marches, led by the general public and by students respectively, as a civic duty to contain the pandemic.
Yet the government does not seem to have acted in the same spirit of solidarity towards the activists. This is illustrated in particular by its treatment of Amazigh organizations. According to a press release of the Congrés Mondial Amazigh, Amazigh communities in Algeria had already mobilized against Covid-19 back in February 2020, before governmental measures were introduced in March, by putting in place ‘vigilance committees’ to limit the spread of the virus in their areas. This autonomous approach, building on the strong cultural and geographical cohesion of many Amazigh, was also prompted by the weakness of the country’s public health infrastructure. The state, however, responded with suspicion, accusing committees of treason and dismantling some village checkpoints using military force.
A history of discrimination
Tamazight languages (known also as ‘Berber languages’. MRG avoids using this term as it is an exonym (chosen by others) and often perceived as derogatory by the communities) were originally spoken from the Canary Islands to Western Egypt (a region called Tamazgha by the Amazighs). Estimates of current Tamazight speakers in Algeria vary significantly, from 17 per cent to 45–55 per cent of the population (taking into account bi- and trilingual speakers) with some regions being heavily Tamazigh-speaking, such as Kabyle. Varieties of Tamazight are often mutually intelligible, and numbers of speakers vary considerably according to the community: in Algeria, Taqbaylit (the Kabyle variety) has millions of speakers, while Chenoua has dozens of thousands of speakers.
The decline of Tamazight in Algeria (mirrored in neighbouring Morocco and Tunisia) was due to the spread of Arabic as the dominant language of religion and mainstream culture, and the rise of French as a prestige language during the colonial era. This erosion was further accelerated by assimilationist policies that even prohibited use of the language: for example, conferences in Tamazight were cancelled. In response, however, the 1980s witnessed a revitalization movement in the region, known as the Amazigh spring. This emerged in a context where, officially, repression of any languages besides Arabic was widespread: the 1989 Algerian Constitution recognized Arabic as the sole national and official language, for instance, while the 1991 Algerian Code on the Use of Arabic Language restricted the use of any language other than Arabic in various circumstances.
A major change came with the creation of the Haut Commissariat à l’Amazighité (HCA) in 1995, placed under the direct supervision of the president of the republic with the objective of promoting the Amazigh language. This followed a year of strikes by students and professors in Kabyle, who were protesting the lack of Tamazight teaching in this predominantly Amazigh region.
A 2002 constitutional amendment subsequently instituted Tamazight as a second national language, echoed in the provision of the 2016 Constitution which, while affirming Arabic as the official language, also states that ‘Tamazight shall also be a national and official language’, with a range of measures to support its promotion and development, including the creation of a dedicated language academy.
Estimates of current Tamazight speakers in Algeria vary significantly, from 17 per cent to 45–55 per cent of the population.
Tamazight learning and education: a casualty of the pandemic
In the 25 years since the launch of the HCA in 1995 and the outbreak of the Covid-19 pandemic, there has been some progress in the rollout of Tamazight teaching in schools in many governorates, yet significant gaps have remained, hampered by limited funding allocations and insufficient planning. The precarious gains of recent years have also been undermined in the wake of the pandemic. To some extent, these challenges were experienced across the country’s entire education system, with primary and secondary schools closed from mid-March 2020 for more than seven months. As for universities, where online teaching remained in place in most cases until December 2020, when the HCA also reopened its doors for adult Tamazight courses, distance learning was undermined by poor internet connections and limited access to laptops and other equipment.
These problems by no means affected Tamazight teaching or the Amazigh people exclusively, as few citizens were left untouched by the crisis, but the long history of marginalization experienced by Tamazight speakers has meant that its impacts have been especially severe. According to Lounes Belkacem, formerly President of the World Amazigh Congress, ‘the state reduced the hours of Amazigh teaching from 3 to 1.5 hours per week. True, most classes were reduced by 50 per cent, however we need to look at the impact. If you divide a big sum into half, there is still a lot left, but if you divide a small one into an even smaller one, there is not much left. So it is not really equitable – everything seems to be made [so as] to suggest that it is not important.’
It is also important to situate these developments against the broader backdrop of rights restrictions that have been rolled out in Algeria during the pandemic. The new Constitution was criticized for the lack of a consultation process around it: though approved in a November 2020 referendum, it was boycotted by Hirak protesters and there was a very low voter turnout. Another major development was the amendment of the Penal Code in April 2020, including a law officially presented as a law against discrimination and hate speech, but which in reality threatens the work of human rights groups and Amazigh activists. The amendments imposed harsh penalties for organizations receiving foreign funding, increased penalties for contempt of public authorities and also added the crime of ‘spreading false news to harm security or public order’.
This came at a moment when several prominent figures in the Hirak, including Amazigh activists, were being imprisoned, such as Yacine Mebarki, sentenced to 10 years in prison in October 2020 (later reduced to one year) for online posts. While the 2020 Constitution celebrates the Hirak movement in its preamble, and the new president, Abdelmadjid Tabboune, has described it as ‘blessed’ on a number of occasions, in reality there has so far been little evidence of democratic change. Two years on from the movement’s momentous beginnings, Hirak activists and journalists continue to be imprisoned. In February 2021, people again took to the streets to mark the second anniversary of the Hirak, while the president announced the release of around 60 people imprisoned for their participation in the movement.
Towards a rights-based approach to the Tamazight language
There have also been recent signs of improvement with regard to the formal learning and use of Tamazight in Algeria. In 2019, for instance, Algeria won the UNESCO King Sejong Literacy Prize for its National Strategy for Multilingual Literacy led by the National Office of Literacy and Education for Adults in Algeria. In the same year, the HCA established a collaboration with the African Academy of Languages, enabling the creation in 2020 of a commission for the Amazigh language under its auspices. The government has also reported an increase in the number of students taught Tamazight and plans have been put in place to expand access for potential learners. In May 2020, the HCA announced the need to develop an Amazigh linguistic map which would help establish a strategy for the development of Tamazight on the ground, with a national consultation scheduled to take place in November before it was postponed on public health grounds.
Yet many problems remain. According to commentators, one of the obstacles in the delivery of good Tamazight teaching is the lack of linguistic planning to accompany the legal guarantees and practical moves, such as allocation of the funding necessary for an increase in the number of teachers in primary, secondary and tertiary education, although there are a number of trained professionals who could take on positions if these were funded; moreover, law no. 2008 on national education, still valid today, provides it as an optional component only (unlike Arabic and French), and reforms have been requested by Amazigh activists and teachers. The secretary of HCA, Si El Hachemi Assad, has spoken repeatedly in support of demands to reform this law and to integrate the teaching of Tamazight into the national education system to give this language ‘its rightful place’ as the mother tongue of many Algerians. He has also noted that in some areas there has been an apparent dip in engagement in Tamazight learning at school. For example, in certain areas such as Jijel, some parents have reportedly protested against Tamazight being taught to their children, demonstrating that the historic stigmatization of the language has not disappeared.
In summary, despite some hard-won progress in recent years and the unavoidable pressures brought on by the pandemic, the ongoing shortfalls in the learning and revitalization of Tamazight in Algeria are also rooted in the ongoing struggles to secure equal rights and opportunities. Although there has been an increasing improvement of official Tamazight education in the last couple of years, this could be seen as part of a larger strategy of concessions, while keeping control centralized and away from the Amazigh communities themselves, which have been targeted by restrictive measures and have been less able to engage in informal community-based language teaching. For all of Algeria’s citizens, but particularly its Amazigh communities, emerging from the shadow of Covid-19 will also require a renewed focus on human rights and inclusion.
Photo: Amazigh women celebrating New Year 2970 in Sahel village, south of Tizi-Ouzou, east of Algiers, 12 January 2020. Yennayer, the first month of the Berber Year, is marked as a national holiday in Algeria for the third time. Credit: EPA-EFE/STRINGER.
-
By Yulian Kondur and Nina Henke
Besides its devastating health impacts, Covid-19 has further marginalized whole communities and is exposing long-standing inequalities. This is especially evident in the area of education. Distance and online learning, adopted in response to the pandemic almost overnight, not only represent a challenge for students, teachers and families but also entail far-reaching social and economic consequences.
According to UNICEF, the crisis has created ‘the largest disruption of education systems in history’ worldwide, affecting nearly 1.6 billion learners.
However, the consequences of closing educational institutions to contain the virus have been especially severe for minority, indigenous and other disadvantaged communities. Not only have learning opportunities been reduced: the lack of social interaction that schools normally provide threatens to undermine any sense of belonging and contribute to their further isolation. While educational institutions should ideally equip learners with effective participation tools, as well as fostering mutual trust and breaking down stereotypes, the crisis has instead isolated minorities further.
One of the largest and most marginalized ethnic minorities in Europe is the Roma community. In Ukraine, as in many countries in Central and Eastern Europe, they face widespread problems, including discrimination, poverty, segregation and under-representation. The pandemic, as well as the official measures put in place to contain it, have hit Roma particularly hard in key areas such as housing and education. As early as April 2020, UNICEF Ukraine had called on the authorities to #LeaveNoOneBehind: even then, it was evident that many Roma children in the country would effectively be left without access to education, particularly given the lack of essential technologies such as personal computers available to them. More than a year later, has anything changed?
While access to education among Roma has long been a concern, a survey by the International Charitable Organization Roma Women’s Fund (Chiricli) of around 450 Roma respondents in six regions of the country highlighted that the basic right to education had been further violated in the wake of the pandemic. Besides a lack of technical equipment (including computers, tablets, phones and access to the internet), the pressures of inadequate housing, overcrowded conditions and stigmatization have made effective remote learning almost impossible for many Roma children, who were generally unprepared for this type of study to begin with. Indeed, the research found that this experience was the norm rather than the exception: only an estimated 8 per cent of those surveyed reported that their children (most of whom were enrolled in higher education) had not experienced any problems attending classes.
73 per cent of Roma people interviewed by Chiricli were not in favour of remote education, pointing in particular to the lack of the necessary technical equipment.
Looking beyond these immediate impacts to other knock-on effects, prolonged remote learning has not only affected those who pursue studies but also their family members. Even when a reliable internet connection and functioning technical equipment are available for students, parents need to assist and guide their children in order for them to perform well in class. These additional obligations often fall to Roma mothers, despite a high level of illiteracy among them and the common necessity to organize children of different age groups simultaneously. Under these circumstances, it does not come as a surprise that negative impressions and attitudes towards distance learning prevail. Amost three quarters (73 per cent) of Roma people interviewed by Chiricli were not in favour of remote education and pointed in particular to their lack of the necessary technical equipment. Troublingly, too, almost one in five (19 per cent) of the respondents reported that they had not received any information on this topic, bringing into question the commitment of Ukrainian social services and other state actors to engage properly with the Roma population. Consequently, Roma non-governmental organizations (NGOs) and mediators have played an important role as one of the main sources of information for communities.
It is readily apparent that distance-learning activities imposed by the state were not successfully implemented for Roma. In particular, the local authorities did not take into consideration how certain measures would disproportionately affect the community’s well-being. When restrictions on movement and other activities were designed, for example, state actors failed to include financial support for those who relied on daily earnings for their survival, and also underestimated the high level of adult illiteracy and the poor living conditions many communities faced. Moreover, until now no other forms of remote education have been developed nor implemented. More than a year on, the national education system still seems unprepared and unable to offer alternative forms of education for Roma children. Yet in response to these pressing challenges, a number of local Roma initiatives have helped bring about positive change. The Romani Early Years Network (REYN) in Ukraine, coordinated by the Roma charitable foundation Blaho, brings together experts in the field of education, social and medical services and parental care. In 2020, a pilot implementation of compensatory educational practices to improve children’s access to education during the pandemic was established in collaboration with local partners. While the state did not introduce any compensation strategies, despite forcing all educational institutions into lockdown from 12 March 2020, various NGOs were able to establish educational practices at local levels to meet the most immediate gaps – ranging from multimedia tools to street schools.
Among these, the NGO Chachimo in Kharkiv conducted digital literacy courses for Roma children and their parents. The training events covered basic computer and smartphone functions, working with distance-learning programmes, text editors, email, search engines and more. The NGO Planet of Kind People in the Odessa region organized a school camp focusing on health and educational programmes for Roma children, including outdoor activities, talks on coronavirus infection prevention, as well as mobile multimedia classes and in-person teaching with a tutor. Likewise, in-person pre-school education was successfully implemented in an interactive and playful way by the NGO Romani Rota in the Cherkasy region. With multicultural activities for young Roma children (4–10 years old) and their parents, the NGO Romano Than in the Kherson region was able to foster the functional development of students’ native language as well as knowledge of Ukrainian, the official state language. Offline classes included the development of writing skills, conversational learning and communication during extra-curricular lessons.
In addition, short-term projects have also demonstrated their ability to add significant value to local communities, as in the case of a 14-day project implemented by the NGO Roma of Ukraine in the Lviv region. Street schools for children living in temporary compact settlements focused on general developmental and educational activities. On top of that, public health information, support to parents and basic literacy development for both children and adults were introduced through a programme that took the living conditions and local needs of the community into account. The same NGO also successfully launched multimedia tools for bilingual education for young Roma children, including five cartoons in four Romani language dialects. The initiative celebrated its success with more than 4,000 views, support from Roma cultural centres in nine regions of Ukraine and official recognition by UNICEF Ukraine.
The NGO Blago, which has kept its centre in Uzhgorod open since June 2020, has also implemented initiatives to support the local Roma population and the youngest students among them. By providing parents with information, offering moral support, facilitating conferences with parents and teachers, and engaging in conversation, the organization has managed to provide guidance to communities through these difficult times. Moreover, the team continues to offer offline learning opportunities for early child development in compliance with all quarantine safety rules and regulations. Their pre-school initiative enables classes of 10 children for 2.5 hours, twice a day, during the week. Before each lesson, every child’s temperature is taken and hands are disinfected. Between the two sessions, the facility is aired out, wet-cleaned and all the desks are disinfected without exception. Additionally, the project also allows outdoor lessons in good weather conditions for up to 10–12 children per class.
Despite initial concerns with regard to children failing to comply with safety rules or experiencing stress due to the new learning conditions, teachers observed careful and responsive behaviour throughout the projects. Moreover, students were grateful for the possibility to learn with their peers and left the classes with smiles on their faces. As Eleanora Kulchar, national coordinator of the REYN-Ukraine network, explains: ‘This period has been especially difficult, and it is even more difficult that we do not know when the quarantine is going to end. However, we understand that our work has become more important in times of a permanent lockdown. Despite all the difficulties, our team does not give up, but finds solutions and continues to work.’
These examples of independent initiatives serve as an inspiration at this time of crisis. However, in order to provide equitable education and learning opportunities for all, the role of the government in funding and implementing meaningful and inclusive policies is more important than ever. While NGOs and community organizations are already delivering invaluable support, they cannot take on the burden of this responsibility indefinitely without adequate assistance from the state.
Special thanks to Halyna Yurchenko, project manager of the NGO Roma of Ukraine ‘TERNIPE’ and project assistant to REYN-Ukraine, who contributed significantly to this case study by sharing best practice examples from the respective regions.
Photo: Children exercising during an informal educational activity linked to the promotion of healthy lifestyles. Berezovka, Odesa region, Ukraine. Credit: Planet of Kind People.
Surveillance and policing
Governments must employ public health strategies that are participatory and rights-based, not repressive and controlling: In many countries, the pandemic has been used to justify the rollout of discriminatory restrictions that have actively hindered an effective response. While the pandemic required swift and unprecedented action from governments across the world, some countries saw the rollout of inequitable and discriminatory policies that created further challenges for poor and marginalized groups. In many cases, these actively targeted minorities, indigenous peoples and migrants with disproportionate measures that were not applied to the rest of the population. Authorities have also cynically used the pandemic as a pretext to crack down on protests and ramp up surveillance of their populations, framing citizens as vectors of the disease to be contained rather than potential victims in need of protection. However, this draconian approach has frequently not only violated fundamental rights but also impacted negatively on public health, in some cases intimidating communities into avoiding testing or treatment for fear of reprisals.
- 01

China: ‘Covid diplomacy’ fuelled by Uyghur oppression
By Michael Caster Throughout 2020, while much of the world was asked to stay home and socially distance, upwards of 1 million Uyghurs continued to suffer mass forced internment in north-western China’s Xinjiang region, also known as…
0 min read
- 02

Iraq: Protesting for human rights in the midst of a pandemic
By Ali Khadr October 2019 marked the start of the largest instance of civil unrest in central and southern Iraqi provinces since 2003. Tens of thousands of people took to the streets to protest corruption, widespread unemployment, a…
1 min read
- 03

Kyrgyzstan: In the wake of Covid-19, the threat to the rights of minorities and other marginalized groups is greater than ever
By Tolekan Ismailova While the pandemic has been experienced globally, many of its impacts have been highly localized, exposing the specific challenges facing different countries. In the case of Kyrgyzstan, the outbreak of Covid-19 has…
1 min read
-
By Michael Caster
Throughout 2020, while much of the world was asked to stay home and socially distance, upwards of 1 million Uyghurs continued to suffer mass forced internment in north-western China’s Xinjiang region, also known as East Turkestan. After the outbreak of Covid-19 in Wuhan and a period of obstructing access to information about its spread, China imposed draconian disease control restrictions on tens of millions of its citizens. But in Xinjiang, the region’s Uyghur and Kazakh populations had already been living in a state of totalitarian control for years.
The UN Committee on the Elimination of Racial Discrimination in 2018 had called Xinjiang a ‘no rights zone’, amid the mass detention of hundreds of thousands of civilians from ethnic and religious minorities. China claims they are merely ‘vocational training centres’, but satellite imagery and first-person accounts tell a horror story of barbed wire, surveillance cameras and armed guards. Many are forced labour camps.
Overcrowding and malnutrition leave inmates highly vulnerable to the spread of infectious diseases: even before the pandemic, former detainees highlighted the prevalence of illness in the camps and the difficulty in accessing adequate medical care. Responding to such concerns in the wake of Covid-19, especially in the early months of the outbreak, social media campaigns gained traction in raising awareness of the suffering of the Uyghurs with hashtags such as #VirusThreatInTheCamps and #WHO2Urumqi, the latter calling for the World Health Organization to send a delegation to the regional capital Urumqi.
Meanwhile, outside the camps, Uyghurs faced another plight. The sudden imposition and harsh enforcement of a Covid-related lockdown in mid-February 2020 made it nearly impossible for Uyghur residents to procure food, medicine and other supplies. As Rights Project (UHRP) at the time, Uyghur-language media, including on Douyin, the Chinese parent version of TikTok, had lit up with disturbing videos and images of residents in danger of starving.
Between 2017 and 2019, more than 80,000 Uyghurs were forcibly transferred from Xinjiang to factories around China, remaining trapped in highly surveilled facilities.
Calls for an independent fact-finding mission to inspect mass forced internment and other widespread human rights abuses over the years, as well as more recently to assess the spread of Covid-19 cases and food insecurity among the Uyghur population, have gone unheeded by authorities who have for years refused all pleas for effective independent investigations of human rights abuses in Xinjiang. Nor have these abuses been confined to Xinjiang alone. Conservative estimates suggest that between 2017 and 2019, more than 80,000 Uyghurs were forcibly transferred from Xinjiang to factories around China. Even far from Xinjiang, they remained trapped in segregated and highly surveilled facilities, in many cases forming part of the supply chains of major global brands.
However, even after Covid-related restrictions emptied factories across China of their Han workers, Uyghurs remained, putting them at heightened risk of infection. Despite the risks, from February 2020, as China’s coronavirus figures were peaking, hundreds more Uyghurs were forcibly transferred from Xinjiang to factories in Hunan, Jiangsu, Jiangxi and Zhejiang provinces. Official reports were given a human face by the many videos posted to Douyin showing Uyghurs being forced onto buses bound for factories across China. At the height of the pandemic, when across the country civilians were quarantined at home for their own protection and many companies had suspended production to prevent transmission of the virus, tens of thousands of Uyghurs were forced to continue working.
At the same time, from early March 2020 onwards, China launched a PR campaign of what has been dubbed ‘mask diplomacy’, shipping medical supplies and personal protective equipment (PPE) around the world as a humanitarian gesture while other nations were struggling with rising coronavirus infection rates. These efforts, no doubt intended to counteract the negativity around the origins of the virus in China, were enthusiastically promoted by Chinese state media and diplomats on social media platforms, including Facebook and Twitter (both blocked in China itself).
According to data compiled by Stanford University, between January and May 2020, 11 English-language Chinese social media accounts issued 3,144 tweets promoting Beijing’s ‘mask diplomacy’.
This online campaign appeared to be focused largely on Europe: according to data compiled by Stanford University, between January and May 2020, 11 English-language Chinese social media accounts issued some 3,144 tweets promoting Beijing’s ‘mask diplomacy’. For all its propaganda, China’s efforts were met with mounting criticism, particularly around the low quality of some of the materials being exported to other countries. However, one of the problems with its ‘mask diplomacy’ that got less attention than it deserved was how some of these masks were being produced. Given just how entrenched Uyghur forced labour is in the entire Chinese supply chain, it is not surprising to learn that some of the companies producing the PPE shipped abroad were tainted.
This was illustrated by a New York Times investigation which revealed that while China’s National Medical Products Administration only listed four companies in Xinjiang producing medical-grade PPE before the pandemic, the number had increased to 51 by the end of June 2020, with at least 17 of them known conclusively to rely on forced labour. These companies claimed they were primarily producing for domestic use. But others that had relied on the Uyghur forced labour transfer programme mentioned earlier, such as one in Hubei Province, were supplying PPE directly to the United States. Further supply-chain analysis revealed that major European distributors OneMed, a Swedish medical supplier, and the European subsidiary of the American pharmaceutical firm McKesson have sourced PPE for European distribution from Chinese producers known for exploiting Uyghur forced labour.
China has also pursued ‘vaccine diplomacy’ through its homegrown Sinovac Biotech vaccine, which has raised other concerns. In Turkey, the first batches of Sinovac were delayed in December 2020, notably as Beijing unexpectedly announced that it had ratified an extradition agreement signed between the two countries in 2017. This led to some speculation about whether China was trying to barter access to its vaccine in exchange for control over Turkey’s Uyghur population. Many have expressed horror at the idea of a formal extradition agreement between China and Turkey, where large communities of Uyghurs reside in exile, fearful that they could be forcibly repatriated to China where they would be at risk of gross human rights violations.
China has overseen a further extension of the repression of its Uyghur population during the pandemic, tightening its hold not only on the millions of civilians within its borders but also those who have managed to seek sanctuary abroad from the state’s persecution.
Photo: Police officers patrol the square in front of Id Kah Mosque in Kashgar, Xinjiang Uyghur Autonomous Region, China. 3 May 2021. Credit: Reuters/Thomas Peter.
-
By Ali Khadr
October 2019 marked the start of the largest instance of civil unrest in central and southern Iraqi provinces since 2003. Tens of thousands of people took to the streets to protest corruption, widespread unemployment, a severe lack of public services and foreign interference in the country. While these issues affect the entire country, they are particularly pertinent to minority areas, and echo minority concerns around participation, accountability and security. Civil society demanded the dismantling of the entire political establishment for its failure to improve living standards for much of the population while reinforcing the narrow political elite’s hold on power and resources.
The resignation of Iraqi Prime Minister Adel Abdul Mahdi in late November 2019 was a significant milestone of the movement, but it was not enough to meet the demands of the protesters. The entrenched political status quo led by the muhasasa system – the quotas established by the United States following its invasion of the country – was being challenged. In response, protesters faced severe crackdowns and attacks with live ammunition, rubber bullets, snipers, tear gas, round-the-clock curfews and internet blackouts, leading to some 669 deaths, 25,000 injuries and 2,800 arrests by January 2021.
Then came the arrival of Covid-19. Iraq recorded its first official case in Najaf on 24 February 2020. Despite the obvious public health dangers posed by the virus, protesters were reluctant to halt the demonstrations. On 11 March 2020, the World Health Organization declared the coronavirus outbreak a global pandemic. Initially, protesters denounced the ensuing government-imposed curfews and prohibitions of large gatherings as a pretext to suppress the civil society movement. After all, a supposed government concern for public health was in direct contradiction to its clear disregard for the lives of peaceful demonstrators. It also would not have been the first attempt to supress protester demands.
Censorship of activists, protesters and journalists in Iraq pre-dated the pandemic. A series of kidnappings and assassinations has plagued the protest movement and these continue. It is believed that more than 60 activists have been assassinated by unknown gunmen, including photojournalist Ahmad Muhanna Al-Lami, who was shot in the back while covering the protests on 6 December 2019. Civil society activist Fahem al-Tai was killed on 8 December 2019 in Karbala after returning from the protests. Female activists have also been targeted. Janat Madhi was gunned down as she returned from a day of protesting in Iraq’s southern city of Basra on 21 January 2020 and Reham Yacoub was killed when gunmen opened fire on her vehicle in Basra on 19 August 2020. The emergence of Covid-19 has not stopped these attacks. On 10 March 2021, Jasb Hattab Aboud was killed after being highly vocal and seeking accountability for the disappearance of his son, Ali Jasb, at the height of the anti-government protests in October 2019. Meanwhile rhetoric to delegitimize the protesters has been widely used by political and religious elites, who have accused them of immorality, and thereby posing a threat to social and religious norms in the country.
A series of kidnappings and assassinations has plagued the protest movement: it is believed that more than 60 activists have been assassinated by unknown gunmen.
The Communications and Media Commission (CMC), an institution that is said to be financially and administratively independent from the government, ordered the closure of eight television broadcasters and four radio stations for three months for breaching regulations, with five other broadcasters also being warned over their coverage of the protests. More recently, the CMC invoked the Media Broadcasting Rules to suspend Reuters’ licence on 2 April 2020 for three months and fined them 25 million IQD (US$21,000), after they published a story claiming the number of Covid-19 cases in the country was higher than shown by government figures. Reuters was accused of relying on unsubstantiated claims and sources to fabricate news about the virus in Iraq, endangering public safety and hindering the government’s efforts to prevent the spread of the virus. The suspension was lifted on 19 April 2020.
In the Kurdish Region of Iraq (KRI), several cases of arbitrary arrests, detention, and prosecution of journalists, bloggers and protesters have also been recorded. In December 2020, protests broke out in the governorate of Sulaymaniyah, despite pandemic-related restrictions. Thousands of public sector workers took to the streets to demand their unpaid wages and, like their fellow demonstrators in central and southern Iraq, they were met with water cannons, rubber bullets and tear gas, killing 10 and injuring 65.
Hemin Mamand, a journalist in the KRI, was arrested after posting a message on Facebook criticizing the Kurdish Regional Government for withholding public servants’ salaries and the Covid-19-related lockdown restrictions. Hemin was detained the very next day, without a warrant by unidentified authorities, information he would later relay on Facebook, for which he was rearrested. In his 15 days of detention, Hemin was only permitted one call to his lawyer and was denied face-to-face access, under the pretext of Covid-19 protection measures.
Activists were no longer protesting for their livelihoods; they were protesting for their lives. For many, Covid-19 was no greater threat than the economic, social and political reality they would face if the protests were not successful. For others, the invisible threat of a virus was not as severe as the blinding effects of gas canisters used to disperse and attack them. The harsh reality was that the increased number of deaths due to disease did not change the circumstances that led the demonstrators to risk their lives in the first place.
In December 2020, thousands of public sector workers in Sulaymaniyah took to the streets to demand their unpaid wages. They were met with water cannons, rubber bullets and tear gas, killing 10 and injuring 65.
In minority areas in Iraq, the threat of ISIS has loomed large. Rather than dampening its resolve, the pandemic seems to have afforded the extremist group opportunity to renew its strategy and intensify its attacks while security forces were distracted. The instability inevitably caused by civil unrest and demonstrations was not an outcome that many minority groups could or would risk in their territories, after ISIS had already exploited such conditions to commit mass atrocities and expel them from their historical homelands.
This is not to say that minorities have not been present and part of the civil society movement. Protesters pride themselves on the political, religious, social, ethnic, gender and ideological diversity of demonstrators – particularly in Baghdad – which they believe lends strength and legitimacy to the movement. Overall, the decentralized nature of the protests and its lack of hierarchy had helped it survive months of repression and brutality. Yet with Covid-19, these characteristics placed the movement and those engaging with it at further risk. While some groups continued to occupy public spaces in a number of cities in central and southern Iraq, many others announced a halt to their rallies in line with the new restrictions.
Nevertheless, significant efforts were undertaken by demonstrators to ensure Covid-safe spaces for protests. For a while, to avoid overcrowding, demonstrators in Baghdad implemented a rotational system in an attempt to keep pressure on the government and ensure the movement stays alive amidst dwindling numbers. Those who remained undertook an active civic service role to fill the gaps left by the government in response to the pandemic. The temporary clinics established by demonstrators in Tahrir Square (the epicentre of the mass protest movement) to treat those wounded in the attacks against them were now being used to distribute face masks, plastic gloves and hand sanitizer. Protesters shared health information in pamphlets and speeches. Some initiated campaigns to sterilize areas of demonstrations while others sprayed public streets with disinfectant. Through such measures, protesters challenged notions that it is the protests, rather than the injustices driving them, that are dangerous.
Recent reports indicated that at least 83 governments worldwide have used the pandemic to justify the violation of the right to free speech and peaceful assembly. The irony of these actions is not lost on Iraqi civil society.
Eventually, however, the pandemic led to the dispersal of the majority of protesters in Tahrir Square, and the protests officially ended on 21 March 2020 as concerns regarding the rampant spread of the virus increased. Organizers vowed to revive the protests should the government fail to make any headway in addressing their demands. Iraqis watched from afar as Covid-19 restrictions were used to forcefully dismantle and ban mass protest movements in Lebanon and Algeria. Recent reports indicated that at least 83 governments worldwide have used the pandemic to justify the violation of the right to free speech and peaceful assembly. The irony of these actions is not lost on Iraqi civil society. Any public health justification for violent disruptions of demonstrations and mass detention is undermined by the very nature of these measures that threaten the lives and freedoms of protesters.
Yet while violent crackdowns and the virus have worked together to physically disperse the protesters from public spaces, the same The use of hashtags such as ‘Iraq is bleeding’ helped gain international attention and condemnation of government crackdowns, while online memorialization of those killed in the protests and assassinations has mobilized civil society across Iraq and strengthened calls for investigation and justice. The digital space created throughout the demonstrations remained available and active as the threat shifted from armed killings to global pandemic. cannot necessarily be claimed for the digital movement that occurred in parallel. As a result of state or militia violence against protesters, online activism has always been an option for those who wished to demand their rights without risking their physical safety. Virtual protests have played a pivotal role in both stimulating the movement and voicing demands to wider communities in the absence of state media coverage.
The pandemic has amplified the economic hardships of Iraqi civil society. A year and a half since mass protests broke out, protesters’ demands remain pertinent and relevant. In April 2021, demonstrators once again began to gather in the southern districts of Iraq to demand their rights. Until real significant economic and political change is realized, the movement will likely continue, despite the twin perils of Covid-19 and state repression.
Photo: Iraqi demonstrators gather to mark the first anniversary of the anti-government protests in Baghdad, Iraq October 25, 2020. Credit: REUTERS/Thaier Al-Sudani.
-
By Tolekan Ismailova
While the pandemic has been experienced globally, many of its impacts have been highly localized, exposing the specific challenges facing different countries. In the case of Kyrgyzstan, the outbreak of Covid-19 has exposed the vulnerability of the country’s dilapidated economic and governance systems. It has also highlighted the perilous state of human rights in the country, particularly for its minority populations – a situation illustrated by the fact that, more than a decade after the tragic inter-ethnic clashes in 2010 that saw almost 500 people killed, its predominantly ethnic Uzbek victims are still seeking justice and fighting impunity.
In response to the pandemic, a national emergency was announced in Kyrgyzstan in March 2020, with stringent restrictions imposed in Bishkek and a number of other cities. As part of the state of emergency, initially in force until 15 April but later prolonged until 10 May, a curfew was introduced and people’s movement was limited, with police checkpoints established to enforce these controls. While to some extent these mirrored measures put in place elsewhere, the implications for the protection of freedom of expression, association and assembly are especially concerning in the Kyrgyz context. Subsequent actions by the government also suggest that security and repression, rather than public health, have been its main priorities in responding to the virus. Throughout, marginalized and discriminated groups such as minorities, women and LGBTQ+ persons have been overlooked or even targeted by the authorities, despite their heightened vulnerability to the pandemic and its social effects.
For many years, civil society in the country has suffered from a narrowing public space, with instances of organizations disbanding, suspending their activities or struggling to secure funding. Staff members are intimidated, detained or assaulted, sometimes even killed. Informal social movements without official approval experience similar threats, as do journalists, academics and bloggers. When they do not suffer from direct repression, they still tend to be affected indirectly through self-censorship and a refocusing of their activities, away from human rights advocacy towards the less contested area of service provision.
From rising homelessness to increased domestic violence, human rights issues have only become more urgent during the pandemic. Yet throughout, despite these pressures, the government has failed to provide adequate assistance to those worst affected, including marginalized groups such as women, the elderly and people with disabilities. In orphanages, mental health facilities and boarding schools for children with special needs in Chui region, for instance, staff reportedly had to sew their own protective equipment and produce their own sanitizing materials. In prisons, too, inmates have not only been denied visits from family members but also from doctors and lawyers: out of around 2,500 lawyers who applied for state authorization to access their clients in prison during the lockdown, only 139 were approved – far fewer than in the pre-pandemic period, when almost all requested visits were permitted.
Out of around 2,500 lawyers who applied for state authorization to access their clients in prison during the lockdown, only 139 were approved.
Instead of focusing all efforts on protecting the civilian population in the midst of an unprecedented health emergency, the authorities have been passing more legislation against civil society, including those working on women’s rights. This renewed repression also included an attack in April 2020 by self-styled nationalists against activists protesting against the abduction and murder of a young woman, Aizada Kanatbekova, with the vigilantes falsely accusing the demonstrators of seeking to promote LGBTQ+ issues — a long-standing target of official persecution and homophobic policies. LGBTQ+ activists have highlighted that homophobic violence against community members has only increased since the pandemic began; as a large proportion of attacks against LGBTQ+ people take place at home, the imposition of quarantine and lockdowns has left many exposed to even greater risks of domestic violence.
Ethnic minorities have also been especially affected during this period. In a submission to the UN Committee on the Elimination of Racial Discrimination in October 2020, the human rights groups ADC Memorial and Bir Duino Kyrgyzstan expressed their concern about the heightened plight of ethnic minorities at a time of social and political instability following mass protests, the president’s resignation and the postponement of parliamentary elections. Ethnic minorities living in crowded settlements have faced additional risks during the pandemic, made worse by the lack of available information about the dangers of Covid-19 and prevention measures. This is because many do not speak the Kyrgyz or Russian languages fluently, lack access to the internet and social media, and follow certain religious and traditional practices that make social distancing difficult. Human rights groups called on the government urgently to consider the specific needs and lifestyles of ethnic minorities to minimize the spread of the virus in these communities.
The perilous state of human rights in Kyrgyzstan was illustrated by the plight of Azimzhan Askarov, a 69-year-old ethnic Uzbek journalist and human rights defender who worked tirelessly to document abuses during the violence in 2010 and was subsequently convicted of complicity in a trial that was widely criticized for its many irregularities. His death in custody in July 2020 was the tragic result of the Kyrgyz government ignoring calls for his release from Kyrgyz civil society, international organizations, heads of state and public figures over many years. While much has changed since the onset of the pandemic, the repression and marginalization of ethnic minorities, human rights activists and other targeted groups has shown no signs of abating.
Photo: A Muslim religious leader from the ethnic Uzbek community in Kyrgyzstan. Credit: Franck METOIS/Alamy.
Hate speech and misinformation
Address the dissemination of harmful rumours and misinformation linking the spread of Covid-19 to minorities, indigenous peoples and other excluded communities: Right-wing and nationalist groups have sought to exploit the fear and confusion brought on by the pandemic to attack marginalized groups. Hate speech and misinformation about Covid-19 have spread as quickly as the virus itself, with disastrous and sometimes deadly effects. Extremists have sought to weaponize the pandemic through the promotion of false narratives blaming particular communities for the outbreak, further endangering their security. Frequently building on old stereotypes and drawing on bad science to justify discrimination, this hate speech has also served to undermine wider public health strategies. These attacks foster division and misinformation at a time when collective action and accurate messaging are more important than ever.
- 01

Argentina: Antisemitism on the rise in the midst of the pandemic
By Carla Torres Thought to number just over 180,000 people today (although some estimates are higher), Jewish people in Argentina have long been victims of hate speech. During the pandemic, however, antisemitic rhetoric against the…
0 min read
- 02

South Africa: In the midst of the pandemic, anti-foreigner sentiment has flourished
By Hamimu Masudi News headlines of violence against immigrants in South Africa started to appear in 2008, when mobs in the country’s economic heartland province of Gauteng, and later KwaZulu-Natal and Western Cape, sporadically…
1 min read
- 03

Sri Lanka: Bad science and the ban on Muslim burials
By Jashan Jegasothy Sri Lanka is no stranger to the harmful consequences of misinformation. In the past decade alone, the spread of misinformation, both online and offline, has been the cause of multiple communal riots which have resulted in…
1 min read
-
By Carla Torres
Thought to number just over 180,000 people today (although some estimates are higher), Jewish people in Argentina have long been victims of hate speech. During the pandemic, however, antisemitic rhetoric against the community in national media increased alarmingly.
The Covid-19 crisis has triggered a proliferation of conspiracy theories and slurs, including accusations of profiteering levelled against Jewish businessmen linked with the production of vaccines and soybean. This rhetoric taps into a long history of stigma and discrimination against the community.
Notoriously, after the Second World War, Argentina served as a refuge for Nazi leaders such as Adolf Eichmann and Josef Mengele. During the military junta’s dictatorship (1976–83), relatives of abducted Jewish community members were subject to extortion by military officers asking for money and properties in exchange for the return of victims, many of whom were already dead. Jewish detainees being held in facilities were often treated brutally and subsequent estimates suggest that more than 12 per cent of those ‘disappeared’ by the regime were Jewish.
Antisemitism did not end with the fall of the junta. Two separate terrorist attacks have been perpetrated against Jewish institutions in Argentina: the bombing of the Israeli embassy in 1992, killing 29 people, followed by an even deadlier attack against the Argentine Israelite Mutual Association (AMIA) in 1994 that resulted in the deaths of 85 people. Both incidents remain unsolved. In 2015, National Prosecutor Alberto Nisman was found dead in his house. Nisman had been due to publish a report into the 1994 attack, which reportedly accused the Argentinian government of complicity in a cover-up.
There have been some positive steps in recent years, including Argentina’s adoption in 2020 of a new definition of antisemitism as ‘a certain perception of Jews that can be expressed as hatred for Jews’.
There have been some positive steps in recent years, including Argentina’s adoption in 2020 of a new definition of antisemitism as ‘a certain perception of Jews that can be expressed as hatred for Jews’. This formulation was developed for those working in local authorities, public administration and the civil service, and subsequently adopted by the Ministry of Foreign Affairs with the overall aim of reducing antisemitism and discriminatory acts in the public sector. Nevertheless, as highlighted by organizations such as the Delegation of Argentine Israelite Associations (DAIA), a variety of manifestations of antisemitism persist in the country today, ranging from xenophobic statements and stereotypes to conspiracy theories and Nazi symbology.
The DAIA has also drawn attention to the proliferation of antisemitism online, in particular linked to the pandemic. Many of these statements accuse Jewish families of demanding preferential treatment when seeing a doctor, controlling the Argentinian government and seeking the expansion of Zionism. In addition, its research uncovered countless conspiracy theories demonizing Jews on social media. In some cases, these adapt old antisemitic tropes to the new reality of Covid-19: for example, in April 2021, tweets by a high-profile businessman who is under house arrest accused several Jewish businessmen of corruption and specifically targeted one Jewish business leader, Hugo Sigman, for his involvement in local production of the AstraZeneca vaccine against Covid-19.
Antisemitic declarations have also appeared in traditional media outlets and from elected officials. In January 2021, Congressman and political leader Pablo Ansaloni accused the Argentine Jewish community of being ‘stateless’, with no respect for or attachment to Argentina, while delivering a presentation about trade unions in Argentina. ‘We are closer than ever, no one will break us’, he said in a public address, ‘because out there, they are like the Jews, who have no homeland and do not know where they are or who they represent.’ Shortly after Ansaloni’s declarations, a Jewish family was savagely attacked in La Falda, Córdoba, with the aggressors allegedly beating the father after intercepting their car following a chase.
For Jewish Argentinians, beyond its immediate health impacts, the pandemic has therefore brought an added threat – the revival of destructive antisemitic stereotypes and falsehoods in a country where memories of targeted violence against the community are still fresh.
Photo: Jewish community members wear face masks as they walk outside a closed store, as Argentina works to organize arrival of a rabbis’ delegation from Israel to keep kosher beef lines going in the midst of the coronavirus disease (Covid-19) outbreak, in Buenos Aires, Argentina May 20, 2020. Credit: REUTERS/Agustin Marcarian.
-
By Hamimu Masudi
News headlines of violence against immigrants in South Africa started to appear in 2008, when mobs in the country’s economic heartland province of Gauteng, and later KwaZulu-Natal and Western Cape, sporadically attacked foreigners and their businesses, leaving close to 60 people dead and displacing thousands more, in the process forcing many back to Zimbabwe, Mozambique and other countries of origin.
Since then, anti-foreigner attacks have been commonplace, reinvigorated by economic hardships and, most recently, by the Covid-19 pandemic. With its economy performing remarkably well in comparison to most of the continent, the country has been attracting people seeking asylum or in search of work opportunities, mostly from Southern Africa but also from elsewhere, such as Nigeria, Somalia and Bangladesh. For many poor black South African communities, still reeling from their experiences of apartheid and who make up most of the country’s large numbers of unemployed, the presence of migrants is viewed as a threat. This perception has only sharpened in the wake of the pandemic, with national unemployment levels rising to almost a third (32.5 per cent) of the population by the end of 2020.
According to some market surveys, a foreign-born resident is more likely to be employed than a South African citizen living in the same neighbourhood – although, crucially, foreigners are also more likely to be employed in precarious or informal sector work than South African nationals. Most commentators conclude that this difference in employment chances informs the widespread belief among South Africans that foreigners are depriving them of employment and other business opportunities – which, in turn, has contributed to periodic waves of deadly xenophobia.
With the onset of the pandemic, violent anti-foreign sentiments are again re-emerging. In September 2020, as part of a movement calling itself Put South Africa First, a group of South Africans took to the streets with banners, shouting that foreigners were taking away their jobs and demanding that they leave the country. Among other measures, the movement called on the government to undertake a citizenship audit, impose service fees on foreign residents and halt the provision of non-essential work permits immediately. The groups driving these anti-migrant sentiments have also spread rumours accusing foreigners of trafficking children and other unfounded allegations. The implications of these coordinated hate campaigns have been felt even beyond South Africa’s border, with previous xenophobic attacks in the country provoking retaliatory attacks in Nigeria and Zambia targeting South African businesses.
For many poor black South African communities, the presence of migrants is viewed as a threat. This perception has only sharpened in the wake of the pandemic, with national unemployment levels rising to almost a third (32.5 per cent) of the population by the end of 2020.
Other practices adopted to control the spread of Covid-19 have also been reported to be discriminatory towards refugees, asylum seekers, migrants, foreign workers and foreign business. This was especially so during the initial days of lockdown, when the government targeted these groups with stringent control measures, as illustrated by the abrupt closure of some refugee centres, mostly without any prompt and decisive safeguards. For some asylum seekers, such moves had immediate repercussions; since they were unable to renew their permits, their bank accounts were frozen, leaving them unable to purchase food and other necessities.
In many cases, government officials have not only failed to challenge xenophobic attitudes but actively encouraged them through their words and actions. Further still, government officials also came under scrutiny for using non-inclusive language in their public messages, a case in point being the tendency of the officials to refer to South African ‘citizens’ instead of ‘all in South Africa’ in their communications around Covid-19, further stoking divisions in the midst of a collective public health emergency.
One particularly egregious instance of this took place in March 2020 when South Africa’s Small Business and Development Minister, Khumbudzo Ntshavheni, deliberately excluded foreign-owned grocery shops from the list of designated essential service providers that could remain open during lockdown. Even though a new directive was issued in April, reversing the minister’s position, the damage had already been done, and human rights defenders castigated her for playing into popular prejudices against migrants in the country. To make matters worse, in the process of implementing the directives, police had used unnecessary force and themselves uttered xenophobic statements. In one instance, Mohamed Surat of Enjeni Spaza told reporters that he and his customers had been pepper sprayed by the police in his shop.
The prevalence of hate speech against migrants in a variety of contexts – South Africa’s media has also been criticized for conveying messages that frequently normalize xenophobia – means that addressing the rise of xenophobia in the country requires a range of social and economic interventions to challenge misinformation and address underlying grievances around poverty and inequality, many rooted in the legacy of apartheid. Though Covid-19 has made these issues more visible, targeted violence against foreigners in South Africa long pre-dates the pandemic and is likely, without adequate measures to tackle it, to continue indefinitely – posing a public health crisis of its own to the millions of migrants and asylum seekers living there.
Photo: Police check asylum papers of an African foreign national refugee in Cape Town, South Africa. Credit: Guy Oliver/Alamy.
-
By Jashan Jegasothy
Sri Lanka is no stranger to the harmful consequences of misinformation. In the past decade alone, the spread of misinformation, both online and offline, has been the cause of multiple communal riots which have resulted in lives, homes, livelihoods and places of worship being destroyed. Minority communities have borne the brunt of these incidents, with no due justice being served. With the advent of Covid-19, misinformation has continued to wreak havoc, this time coupled with bad science, further entrenching discrimination against minority communities.
At first, the government of Sri Lanka appeared to respond well to the pandemic. The measures included a strict strategy of detecting cases, identifying close contacts, enforcing quarantines, travel restrictions, and isolating certain villages that showed an increase in positive cases. The military-led strategy, headed by the army commander who was appointed to lead the presidential Covid-19 task force, focused on minimizing human movement with a nationwide curfew implemented from 20 March 2020 that would continue for a period of three months.
But while these measures helped flatten the curve during the early part of the year, there were simultaneous shortcomings. For instance, the fact that military personnel were put in charge of almost every sector involved on the frontlines meant that decisions which should ideally have been made by qualified health professionals were instead being led by generals and strongmen. Furthermore, there was no safety net in place for low-income and informal workers who suddenly found themselves out of work during lockdown. These issues, however, would not be the only concerns but merely serve as stepping stones for even greater issues ahead, many of them stemming directly from the government itself.
Since the end of the 30-year civil war in 2009, Sri Lanka’s Muslim minority community, comprising some 10 per cent of the country’s population, has been subjected to routine Islamophobia by media outlets and exploited by nationalist politicians to garner votes. This had led to increased discrimination against Muslims, at times even spilling into violence: for example, a series of anti-Muslim attacks have taken place in recent years, including Aluthgama in 2014, Gintota in November 2017, Ampara in February 2018, Digana and Teldeniya in March 2018, and across much of the Northwestern Province in April and May 2019 following the Easter bombings. And now, during the pandemic, Islamophobic sentiments and actions have again been encouraged by those in power as a distraction from the economic and social fallout brought on by the government’s mishandling of the Covid-19 crisis.
While anti-Muslim groups in Sri Lanka have frequently sought to stigmatize different elements associated with the community, from face coverings to halal meat, this time the focus has been on burial – a custom carried out by both Muslims and Christians, in contrast to the cremations practised by the country’s Buddhist majority. In April 2020, a gazette notification was released by the government mandating cremation as the only acceptable method of disposing of the remains of those who succumb to Covid-19. Despite World Health Organization (WHO) guidelines providing for burial as well as cremation, the authorities presented it as a public health risk. With this move, bad science partnered with religious prejudice to prevent Muslims and other minorities from practising this basic religious right – and contributed in the process to the notion that their practices somehow aided the spread of the virus.
This new regulation prompted immediate outrage among Muslims, Christians and human rights groups. The gazette notification was challenged via Fundamental Rights Applications by civil society as well as Muslim and Catholic families in the Supreme Court. The petitions demanded evidence for the claims about burials contaminating ground water. However, the Supreme Court refused to grant leave to proceed, thus effectively dismissing the petitions. Those protesting the ban, some of whom themselves had seen loved ones forcibly cremated, questioned why Sri Lanka was almost alone in the world in prohibiting burials in the name of public health. For many, it seemed that discrimination, rather than medical protocols, were guiding the government’s response.
This was further confirmed when the Ministry of Health, having commissioned an expert committee of microbiologists and virologists in December 2020 to revisit its policies, then simply ignored the panel’s findings that the bodies of Covid-19 victims could in fact be safely buried as well as cremated. Despite UN human rights experts again urging the Sri Lankan government in January 2021 to end its policy of forced cremation, citing that it ‘amounts to a human rights violation’, the controversial mandatory order to cremate would only be reversed in February 2021, almost a year on from the start of the pandemic. The move was reportedly motivated at least in part to ensure support from the Organisation of Islamic Cooperation (OIC) bloc ahead of a crucial vote at the 46th Session of the UN Human Rights Council.
By then, countless bodies had been cremated unnecessarily against the wishes of their families, including the widely publicized case of a 20-day old infant who was forcibly cremated in December 2020 despite the express objections of his grieving parents. And the government’s subsequent policy, announced at the beginning of March 2021 shortly after the ban on burial was reversed, was still deeply discriminatory: Muslims and Christians could now bury their dead, but only in a designated plot on the remote island of Iranathivu, some 300 kilometres from the capital Colombo. The move faced much opposition from locals in the area, with protests that ultimately forced the government to find alternative sites. The first two bodies were eventually buried in the Ottamavadi area in the eastern Batticaloa district after two Muslim-dominated local councils came forward to provide the burial site.
The government’s stigmatizing policies have also helped contribute to a surge in hate speech against Muslims and other minorities during the pandemic. Research by the National Christian Evangelical Alliance of Sri Lanka, analysing some 103 incidents of published hate speech between March and June 2020, found that 30 per cent of the incidents targeted Christians while 58 per cent targeted Muslims, with burials included as one of the issues apparently driving the increase in anti-Muslim rhetoric. Despite hate speech laws being prevalent in the country, no action has been taken by authorities to protect minorities. It remains to be seen whether Sri Lanka’s vibrant, multicultural and ethnically diverse population can be brought together through a collective effort to manage the virus. The pandemic is a huge hurdle that can only be crossed if Sri Lankans from every caste and creed unite together.
Photo: Sri Lankan Muslims tie white ribbons on a fence at a cemetery during a protest against ‘forcible cremation’ of Covid-19 victims in Colombo, Sri Lanka, 23 December 2020. Credit: EPA-EFE/Chamila Karunarathne.
Conflict
Include a clear conflict prevention component in any global pandemic strategy to prevent a surge in violence: In many countries, the targeting of minorities, indigenous peoples and other marginalized groups has escalated in the midst of the crisis. Early on there were hopes that, given the overwhelming need for collective action to counter the universal threat posed by the pandemic, it might encourage warring parties to suspend hostilities and even enable shared cooperation between them. Yet in many cases, armed groups and militias have actively exploited the crisis for their own ends – particularly where growing political and economic pressures have further undermined already unstable societies. Whether orchestrated by governments, paramilitary factions or terrorist organizations, ethnic cleansing, land grabbing and forced displacement have continued throughout the unfolding disaster of Covid-19, frequently targeting minorities, indigenous peoples and migrants. For many communities, this ongoing violence has been as deadly a threat as the pandemic – and, if not effectively contained, could persist long after the virus has been brought under control.
- 01

Myanmar: For minorities, Covid-19 deepens the effects of conflict
By Sam Stubblefield In the first weeks of the pandemic, there were encouraging signs that Myanmar was being proactive in its Covid-19 response. On 30 January 2020, ahead of most countries in the world, the government created a…
0 min read
- 02

South Caucasus: In the midst of the pandemic, Nagorno-Karabakh’s long-standing conflict shows no signs of abating
By Shorena Kobaidze In the South Caucasus, the outbreak of Covid-19 in 2020 occurred alongside the revival of long-standing ethnic conflicts over the territory in Nagorno-Karabakh. A six-week war between Azerbaijan and Armenia over the…
1 min read
- 03

Global: Weaponizing the pandemic: The impact of Covid-19 in conflict situations
By Miriam Puttick At the outset of the pandemic, the rapid spread of Covid-19 from country to country raised immediate alarm over the catastrophic impact it could have in conflict-affected states, where civilians already suffering from the…
1 min read
-
By Sam Stubblefield
In the first weeks of the pandemic, there were encouraging signs that Myanmar was being proactive in its Covid-19 response. On 30 January 2020, ahead of most countries in the world, the government created a ‘National-Level Central Committee for Covid-19 Prevention, Control and Treatment’ in an effort to get ahead of the virus.
Despite these early efforts, the national-level body which came to have ultimate responsibility for Myanmar’s Covid-19 response — the ‘Coronavirus Disease 2019 Containment and Emergency Response Committee’ — was heavily stacked with military representatives and had a mandate in many ways more focused on security than public health.
The reality of the country’s decades-long civil wars and patchwork of health system governance has meant simultaneously that the central government does not have the capacity to provide adequate health services across the entire country — notably in many border regions, important during a pandemic — and that long-standing mistrust makes cooperation even harder. While authorities in Myanmar announced a ‘no one left behind’ approach to their Covid-19 response, for many citizens access to the central government’s health system was limited or non-existent long before the pandemic began.
Historically, Myanmar’s highly centralized health system has often neglected the diverse needs of ethnic minority populations: health staff from majority areas are typically posted to far-away territories with little understanding of the local needs, cultures and languages. Health infrastructure in ethnic minority areas is underfunded and people living in areas controlled by ethnic armed organizations, especially those fleeing armed conflict, rely on the health services provided by these groups and ethnic health organizations. For hundreds of thousands of internally displaced people (IDPs) stranded in camps in Karen, Rakhine, southern Chin, Kachin and northern Shan states, these are the sole providers of health care.
Ethnic armed groups and health care organizations have implemented a wide range of Covid-19 interventions in conflict areas and territories outside of government control. These local-level responses include community-managed checkpoints and health checks, quarantine centres for travellers, health referrals for those potentially infected, local needs assessments, distribution of personal protective equipment and dissemination of public health information in minority languages. At this time of shared crisis, the importance of this work should be recognized and supported by the Myanmar government and by international donors — yet in practice, these groups have received little support from international donors and have been overlooked by authorities in Myanmar itself. Indeed, in some cases the central government and military have actively disrupted their response efforts.
For the Myanmar military, it seemed that the outbreak was viewed as a strategic opportunity rather than a collective threat. While the number of confirmed Covid-19 cases steadily rose through late March and April 2020, the Myanmar military continued offensives in Rakhine, southern Chin, Karen and northern Shan states. At a time when all focus should have been on addressing the pandemic, people living in ethnic minority areas have had to deal with troop movements, unwanted military road-building projects and fighting that has displaced thousands of people.
To make matters worse, government soldiers were also actively disrupting local Covid-19 response activities in ethnic states, especially those delivered by armed groups. In Shan state, for example, the Restoration Council of Shan State (RCSS) implemented numerous Covid-19 prevention efforts in their territory, including establishing health checkpoints staffed with medics and distributing public health information in Shan language. Yet in April 2020, despite it being a recognized signatory to the Nationwide Ceasefire Agreement, the Myanmar military attacked RCSS soldiers accompanying medics on Covid-19 work and warned local Shan villagers not to accept medical treatment from them. Though the government subsequently promised in June 2020 that it would support RCSS’s Covid-19 response, tensions and military disruption continued on the ground.
While authorities have pursued similar policies elsewhere — in Karen State, for example, the military physically destroyed a number of Covid-19 screening checkpoints established by the Karen National Union and ordered the closure of others — these issues are most pronounced in Rakhine and southern Chin states, where armed conflict has raged throughout the pandemic. The fighting between the Myanmar military and Arakan Army (AA) has in fact intensified in parallel to the unfolding pandemic: on the same day Myanmar announced its first confirmed Covid-19 case the AA was designated a terrorist organization, presaging an increase in the frequency and severity of offensives against it. The expansion of armed conflict in Rakhine state at the same time as the virus was spreading significantly impeded the ability of civil society organizations and international humanitarian agencies to provide a comprehensive response to local people, including many IDPs. Meanwhile, the military’s tactical mobile internet shutdown disrupted people’s access to information on the pandemic. The very real threat of violence — a World Health Organization (WHO) driver was shot and killed while delivering test samples in the first phase of the pandemic, for instance — further obstructed health workers. The pandemic was also used as a pretext for soldiers and police to harass, extort from and assault Rohingya people living in IDP camps.
The emergence of Covid-19 could have been an opportune moment for the Myanmar government to expand cooperation with the existing parallel health systems in ethnic minority areas and build a more effective decentralized health structure to address the pandemic. It could even, perhaps, have offered the possibility of at least a temporary cessation of hostilities as the country rallied to contain the virus. Instead, the military has used the pandemic as a pretext to escalate its use of force, a process that arguably culminated in its February 2021 coup. With the arrest of State Counsellor Aung San Suu Kyi, the killings of hundreds of protesters and the detentions of thousands of others, maintaining power rather than protecting public health appears to be the main priority.
Photo: Members of the Rohingya community gather at the Thet Kel Pyin internally displaced persons (IDP) camp in Sittwe, Rakhine State, Myanmar. Myanmar’s military seized power and declared a state of emergency for one year after arresting State Counselor Aung San Suu Kyi and Myanmar President Win Myint in an early morning raid on 01 February 2021. Credit: EPA-EFE/NYUNT WIN.
-
By Shorena Kobaidze
In the South Caucasus, the outbreak of Covid-19 in 2020 occurred alongside the revival of long-standing ethnic conflicts over the territory in Nagorno-Karabakh. A six-week war between Azerbaijan and Armenia over the long-disputed territory left more than 5,000 people dead and displaced tens of thousands. Following a protracted conflict in the early 1990s between Armenia and Azerbaijan, formally ending with a peace agreement in 1994, Nagorno-Karabakh – despite remaining formally Azerbaijani territory – was in practice a de facto autonomous territory. With hundreds of thousands of ethnic Armenians fleeing elsewhere in Azerbaijan and the simultaneous departure of many ethnic Azeris from the region, its population has since then been overwhelmingly Armenian.
After years of sporadic border clashes, however, outright conflict broke out in September 2020 between Armenian and Azerbaijani forces, culminating in a decisive military victory for the latter. Official estimates show that at least 140,000 civilians were displaced by the fighting, including more than 40,000 into Armenia, amidst widespread destruction of homes, schools, churches and cultural heritage, as well as other serious human rights abuses. While the terms of a Russian-brokered truce leave the future of Nagorno-Karabakh undecided for now, much of the surrounding areas captured by Armenian forces in the previous conflict are under Azerbaijani control. The conflict has also further destabilized the geopolitical climate in South Caucasus, provoking demonstrations and a political crisis in Armenia alongside the resurgence of a triumphant nationalism in Azerbaijan.
This conflict took place in the midst of a global pandemic that has left no country untouched. In Nagorno-Karabakh, the virus, relatively well contained in previous months, spread rapidly through the population as the mass displacement of civilians forced them into close confinement in hazardous, overcrowded conditions. This situation was mirrored in Armenia where the impact of Covid-19 has been severe, particularly following the outbreak of fighting, with an eightfold increase in reported infections during the conflict. An influx of tens of thousands of displaced civilians from Nagorno-Karabakh placed further pressure on its overstretched health system.
In immediate terms, there is little hope that the ceasefire on its own will be a sufficient basis for lasting peace in the region — not while old storylines remain entrenched on either side. The only groups challenging these nationalist narratives are civil society actors in both countries, yet their situation is precarious and contested. In Azerbaijan, a government-led crackdown forced many civil society actors and human rights defenders to cease their activities, with authorities reportedly exploiting Covid-19 restrictions to detain or silence opposition activists. In Armenia, on the other hand, following the peaceful Velvet Revolution in 2018, many civil society representatives and activists took positions in the new government. While this saw an improvement in the public perception and status of civil society organizations, Armenian society has nevertheless become highly polarized between those with liberal views who largely support the new government and supporters of the old regime. Reactionaries in the latter camp have repeatedly depicted these organizations as ‘grant eaters’ or ‘Sorosians’, accusing them of undermining national values and furthering international agendas. These domestic divisions significantly curtail the ability of Armenian civil society actors to forge links and promote dialogue with their counterparts in Azerbaijan.
At least 140,000 civilians were displaced by the fighting, including more than 40,000 into Armenia, amidst widespread destruction of homes, schools, churches and cultural heritage.
Notwithstanding the cessation of hostilities in November 2020, the implications of the recent fighting are also being felt not only in Armenia and Azerbaijan, but also in neighbouring Georgia, where the pandemic has been accompanied by political turmoil in the wake of its October 2020 elections. As the most ethnically diverse state in the South Caucasus, Georgia has long been home to many ethnic groups including sizeable Azerbaijani (6.3 per cent) and Armenian (4.5 per cent) minorities. Historically, both communities have coexisted peacefully and interacted extensively through family ties, networks and civil society associations represented equally by both groups in the various provinces where Armenians live next to Azerbaijanis. This has been aided by the relatively supportive environment in Georgia itself: since its independence, the country has made great progress in creating a policy framework that promotes minority inclusion.
But despite the state’s efforts aimed at decreasing the gap between majority ethnic Georgians and minority Azerbaijani and Armenian populations, the outcomes are not straightforward — and risk being further complicated by the deteriorating relationship between Armenia and Azerbaijan. Many members of ethnic minorities still report feeling marginalized as members of Georgian society. The general consensus among decision-makers is that the main challenge to overcoming the continued economic disparities between different groups is language, given that the inability of most of these minority populations, particularly those aged over 30, to speak Georgian hinders their ability to integrate economically, politically and socially into Georgian life. Fluency in Georgian among minorities is concentrated in the capital and other regions of the country with mixed populations, while fluency in more remote regions with monoethnic minority populations is much lower: for instance, approximately 83 per cent of Azerbaijanis in Kvemo Kartli and 72 per cent of Armenians in Samtskhe-Javakheti do not speak fluent Georgian.
Fluency in Georgian in more remote regions with monoethnic minority populations is much lower compared to large cities: for instance, approximately 83 per cent of Azerbaijanis in Kvemo Kartli and 72 per cent of Armenians in Samtskhe-Javakheti do not speak fluent Georgian.
The sentiment among a significant number of ethnic Georgians is that, despite numerous opportunities for language courses offered to them, minorities are simply not interested in learning. This, of course, overlooks the wide-ranging impacts that history, geography and inequality have played in perpetuating these barriers, instead placing the burden of addressing these obstacles squarely on the communities themselves. Decision-makers often do not fully understand the problems and challenges faced by minority populations because they do not consult with these groups. Furthermore, as identity in Georgia has become increasingly defined by affiliation to one’s homeland, mother tongue spoken and religious affiliation, there is a danger that an ‘us and them’ mentality around majority–minority relations could become established in future. Such an attitude not only ignores the country’s diversity but can also lead to minorities being regarded as a security or social threat, further marginalizing them and exposing them to discrimination, hate speech and nationalism. These are forces that have already forced many members of minorities from the countries in the South Caucasus to migrate on account of their ethnicity.
Destabilization, political crises and deepening ethnic divisions in the South Caucasus have only been exacerbated by the Covid-19 crisis. During the pandemic, as poor and marginalized communities risk becoming even poorer and more marginalized, inclusion, reconciliation and a respect for minority rights are more important than ever, as integral a part of assuring the future stability and well-being of the region as public health and social welfare protections. Understanding and removing the constraints to the development of peace building processes will require renewed efforts and dedication to ensure opportunities, equality and basic services for all, regardless of whether they belong to minority or majority populations.
Photo: Children approach a rocket case in a field near the village of Taghavard in the region of Nagorno-Karabakh, January 11, 2021. Following the military conflict over Nagorno-Karabakh and a further signing of a ceasefire deal, the village was divided into two parts: the Azeri forces stayed in the upper western end and those ethnic Armenians who did not flee live now in the east, reinforced by armed units. Picture taken January 11, 2021. Credit: REUTERS/Artem Mikryukov.
-
By Miriam Puttick
At the outset of the pandemic, the rapid spread of Covid-19 from country to country raised immediate alarm over the catastrophic impact it could have in conflict-affected states, where civilians already suffering from the ravages of war would be left defenceless against a deadly and highly contagious virus.
These concerns led UN Secretary-General António Guterres, on 23 March 2020, to issue an unprecedented call for a global ceasefire, announcing that it was time ‘to put armed conflict on lockdown and focus together on the true fight of our lives’. He called on armed actors around the globe to immediately pause hostilities in order to open opportunities for the passage of aid and enable humanitarian actors to mount a coordinated response to the virus.
The Secretary-General’s urgent plea points to the reality that in many conflict situations, protracted fighting between armed actors has had devastating effects on public health. The erosion of humanitarian norms in several current conflicts has led to repeated attacks on health care facilities and personnel over the years, leaving them weakened and ill-prepared to deal with a public health emergency on the scale of a pandemic. In Syria, according to the non-governmental organization (NGO) Physicians for Human Rights, as of March 2021 there have been at least 599 attacks on hospitals and other health care facilities since the beginning of the conflict in 2011, mostly carried out by pro-government forces, as well as 930 killings of medical professionals. This violence has also had a knock-on effect in forcing many others to flee the country, with as many as 70 per cent of medical workers now believed to have left Syria. In Yemen, meanwhile, barely half of its hospitals and clinics are operational, and about a fifth of the country’s districts do not have a single doctor.
The rationale for the Secretary-General’s ceasefire proposal was compelling and critical – but for the most part, the call went unheeded. While armed actors in a few conflict situations announced limited ceasefire agreements in response to the UN’s call, these did not lead to any significant decrease in levels of fighting at the global level. Available data suggests that at least 21,347 people were killed in conflict between 1 July and 12 September 2020, including more than 5,800 civilians who were directly targeted. In some cases, hostilities actually intensified despite the presence of ceasefires. In Yemen, although the Saudi-led coalition announced a unilateral ceasefire on 8 April, it was seen as a media ploy by the rival Houthi armed group, and attacks continued on all sides. According to the Yemen Data Project, between 9 and 30 April alone, the Saudi-led coalition carried out at least 83 air raids and up to 356 individual strikes. In Libya, fighting also escalated between March and April, with the Haftar-led Libyan National Army (LNA) ramping up its shelling operations on Tripoli and Government of National Accord (GNA) forces making advances into new areas.
In April 2020, using Covid-19 as a pretext, Houthi forces forcibly expelled thousands of Ethiopian migrants from al-Ghar, a migrant settlement in Saada governorate, destroying over 300 tents and houses in the process.
Despite the continuation of hostilities, it is difficult to tell what the consequences have been for the pandemic. Available epidemiological data shows that Covid-19 case counts and mortality levels are lower in many conflict-affected states in comparison to wealthier countries in Europe and North America, but these figures are almost certainly underestimated due to lack of testing capacity and sometimes deliberate under-reporting of infection levels. In Afghanistan, Somalia and Yemen, satellite imagery of burial sites, as well as anecdotal evidence from gravediggers, suggest abnormally high death rates compared to pre-pandemic levels.
Yet, it is impossible to determine how many of these deaths are directly Covid-induced, and how many are the result of other factors. For civilians in conflict-affected states, the most deleterious effects of the pandemic may lie in the social and economic devastation it has caused, rather than in the consequences of infection itself. The global recession caused by the pandemic has compounded the destructive effects of conflict by restricting earning opportunities, disrupting the flow of commodities, driving food prices up and exacerbating poverty. The UN predicts that the number of people facing food insecurity will have doubled to 270 million in eight countries by the end of 2021. Yemen, which was already on the brink of famine due to the Saudi-imposed blockade of its borders, has seen a 20 per cent fall in remittances, an importance source of income for many Yemenis. In Syria, the outbreak of Covid-19 has also exacerbated the country’s economic distress, with more than 80 per cent of the population now living below the poverty line.
These developments have hit already vulnerable groups, such as women, children, minorities and displaced persons, the hardest. For example, members of Yemen’s Muhamasheen minority, already suffering from caste-based discrimination and poverty, are often ineligible for food distribution and other forms of humanitarian aid since they fall outside of tribal structures. Anecdotal reports suggest that many Muhamasheen have also been denied service by health care workers due to fears of Covid-19. In Iraq’s northern Kurdistan region, nearly 40 per cent of registered internally displaced persons (IDPs) are Yezidis, Christians or members of other minorities. Many cannot return to their areas due to the destruction caused by the conflict with ISIS and are living in overcrowded camps with poor sanitation and limited access to health care.
Available data suggests that at least 21,347 people were killed in conflict between 1 July and 12 September 2020, including more than 5,800 civilians who were directly targeted.
Another consequence of the pandemic has been a significant drop in global humanitarian aid flows. Many of the countries mentioned are highly reliant on international aid, a need which has only increased as a result of the pandemic. Yet, donor countries have redirected their budgets to their domestic pandemic responses, reducing the amounts they spend on international aid. In March 2021, the UK government slashed its yearly aid to Yemen nearly in half (£87m compared to £164m the previous year), stating that ‘recent global challenges’ had ‘meant a difficult financial context for us all’.
Making matters worse, armed actors have frequently intercepted humanitarian aid intended for Covid-19 response, using it as leverage for political gain. In Syria, the government has prevented vital supplies from reaching opposition-held areas and has also blocked humanitarian workers and supplies from passing into north-east Syria in order to undermine the authority of the Kurdish-led administration in the region. In Yemen, the Houthis have repeatedly blocked World Health Organization (WHO) shipments arriving in the port of Hodeidah in order to use them as leverage in other negotiations. Similarly, the United Arab Emirates (UAE) -backed Southern Transitional Council, which controls the city of Aden, has prevented the internationally recognized government from accessing Covid-19 equipment sent by the WHO in order to bolster its own status as the de facto authority in the city. The fragmentation of territorial control in conflicts such as these, with overlapping jurisdictions held by different armed actors, adds a further layer of complexity for civilians struggling to access much-needed aid.
These patterns point to a larger trend that has characterized the response to the virus in conflict situations: the weaponization of the pandemic for political gain. In Syria, the government has attempted to distract from its own ineffectual response to the virus by blaming the pandemic on the US while praising the response of its allies Russia, Iran and China. In Yemen, the Houthis have scapegoated African migrants and international aid workers as carriers of the virus, while inflating their own success in controlling infection levels in the areas under their control. In April 2020, using Covid-19 as a pretext, Houthi forces forcibly expelled thousands of Ethiopian migrants from al-Ghar, a migrant settlement in Saada governorate, destroying over 300 tents and houses in the process. The Houthis have also used the pandemic to bolster recruitment to their forces, deploying slogans such as: ‘It is better to die a martyr in heroic battles than to die at home from the coronavirus.’
The refusal of armed actors to heed the call for a global ceasefire thus represents a missed opportunity to reach common ground and alter the course of many conflicts worldwide. The full impact of these decisions on civilians remains to be seen. While the continuation of hostilities has exacerbated the day-to-day suffering of civilians, the ineffectual and politicized response to the pandemic has also eroded the legitimacy of government and non-state armed actors alike. The resulting breakdown of social trust, which is recognized as a major driver of conflict, could continue to fuel violence even after the end of the pandemic.
Photo: Muhamasheen women sit together in Sana’a, Yemen. Credit: EPA / YAHYA ARHAB.
Migration and displacement
Ensure that humane migration policies remain at the heart of the pandemic response, in line with international human rights standards and public health protocols: Many countries appear to have used the crisis as a pretext to impose harsher restrictions on refugees and migrants, leaving them even more exposed to the threat of the virus. Many measures imposed in the wake of Covid-19, such as border closures, mass quarantines and the suspension of asylum claims, have implicitly framed migration as a threat to public health. This approach, while favoured by governments with an established anti-migrant agenda, has placed already vulnerable groups in even greater danger by forcing them to remain in cramped, unsanitary environments such as camps and detention centres. The subsequent waves of infections among refugee and migrant communities, though often employed by right-wing groups to further stigmatize them, have in fact only reinforced the need for a more progressive approach to migration that favours inclusion and integration over penalization and containment. Ensuring equitable access to health care and other rights, such as education and legal employment, will not only support the management of Covid-19 but also create better social and economic outcomes for refugees and migrants as well as host countries.
- 01

Europe: Refugee rights at a standstill: border closures, pushbacks and discrimination in the wake of Covid-19
By Anna Alboth We have been visiting places in Europe touched by the topic of migration for years. Re-visiting the same places, discovering new hotspots, but always staying in touch with people we met: refugees, migrants and asylum-seekers, but…
0 min read
- 02

Spain: As the pandemic bites, growing numbers of refugees and migrants risk the dangerous Atlantic crossing to the Canary Islands
By Anna Alboth ‘Maybe you can work remotely during Covid-19, but in my country, already before the pandemic, half of the population was jobless’, says Adama, a 25-year-old man from Senegal. He arrived in Tenerife, one of the Canary Islands,…
1 min read
- 03

Sudan: As the refugee and IDP crisis escalates, Covid-19 is bringing new woes
By Emily Bauman Despite the best efforts of humanitarian actors in Sudan, refugees, migrants and other displaced people in the country are struggling amidst the dual effects of the coronavirus and renewed violence. For the 1 million…
1 min read
-
By Anna Alboth
We have been visiting places in Europe touched by the topic of migration for years. Re-visiting the same places, discovering new hotspots, but always staying in touch with people we met: refugees, migrants and asylum-seekers, but also NGO workers.
It is always difficult. The feeling of compassion, anger and helplessness is overwhelming, whether you are talking with people on the move in Greece, in Bosnia or in Spain – their situation every year just gets increasingly complicated. And just when you think that nothing can get any worse, along comes Covid-19.
This photo-story is a longer analysis of how the pandemic has placed increasing pressures on refugees and migrants across Europe through heightened border restrictions, suspension of asylum processing, discriminatory restrictions and other measures.
You will see there are no differences between locations at European borders, along the route or in the destination countries: conditions have worsened everywhere.
It is clear that the pandemic has highlighted many gaps in the refugee system across Europe, but it is disturbing to see how some governments have taken advantage of the crisis to push through legally dubious, hardline migration policies under the pretext of public health concerns – measures that could stay in place long after the Covid-19 outbreaks subside.
We found 21 reasons to worry.

Boat after the arrival from Morocco, in the port of Arguineguín, Gran Canaria, Canary Islands. Credit: Karol Grygoruk/RATS Agency. The Canary Islands is a strong example of how Covid-19 has driven an increase in arrivals in some areas. According to a survey by Mixed Migration Centre between April 2020 and January 2021, of almost 5,000 asylum seekers and migrants, almost 50 per cent said Covid-19 was a factor in their decision to leave home.

Boys from Mali in Puerta de la Cruz, Tenerife, Canary Islands. Credit: Karol Grygoruk/RATS Agency. There were disproportionate restrictions on freedom of movement imposed on refugees in Europe. For example, in Greece, residents of Moria camp were allowed to go out only for three hours every week. On the Canary Islands, they were blocked from the mainland and in Italian Trieste, people faced a ban on leaving the city.

Eleonas, refugee camp just out of Athens in the lockdown, Greece. Credit: Karol Grygoruk/RATS Agency. Many countries introduced lockdowns in the camps, even while opening borders for tourists. In Greece, Bosnia and Malta, Covid-19 was an excuse to keep people in the camps, even without positive cases for months. The Council of Europe published a report after visiting Malta, accusing the government of breaking international law and flouting European values by prolonging the detention period several times.

Colegio de Educación Especial (CEIP) Leon, school facilities at Gran Canaria, Canary Islands. Credit: Karol Grygoruk/RATS Agency. Even before the virus reached Europe, reception centres in Belgium, France, Greece, Italy, Malta, and Spain were operating near or above maximum capacity due to a years-long lack of structural investment. The shortage of reception spaces made it difficult to comply with social distancing guidelines. Some EU states turned to ad hoc housing solutions, enforcing lockdown in difficult living conditions – without access to water, sanitation or sufficient room to socially distance.

Access to the motorway, leading to the port in Calais, France. Credit: Karol Grygoruk/RATS Agency. According to UNHCR, during the first wave of the pandemic 168 countries closed or partly-closed their borders. 90 of them still have not made any exception for refugees. Reaching somewhere that could serve as a safe haven has become even more important for many individuals, yet barriers remain: for example, Chechens on the Polish-Belarusian border could not apply for asylum because they could not take the border train.

A family at Victoria Square, Athens, Greece. Credit: Karol Grygoruk/RATS Agency. While a small number of unaccompanied children have been transferred to Germany and Luxembourg from the Greek Islands in 2020, resettlement, relocation of minors and repatriation programs were suspended, which led to some people spending weeks homeless.

Men from Senegal, waiting for the opportunity to go to the police station to apply for asylum, in a temporary facility in hotel Puerto Calma, Gran Canaria, Canary Islands. Credit: Karol Grygoruk/RATS Agency. Everywhere on the refugee route, at least for some weeks, government offices were closed or reduced their services. Legal support, asylum applications, passports, translations – all were stopped, even if waiting times were already very long before the pandemic. Some services have still not resumed.
Asylum claims in EU countries dropped by 31 per cent in 2020. Longer waiting periods increase stress for people in vulnerable situations, especially for people who are homeless or do not have access to social benefits.

Mobile phone charging station, Grande-Synthe settlement, close to Dunkirk, France. Credit: Karol Grygoruk/RATS Agency. After closing the services, there is also less data on migration and movement. In the UK, the International Passenger Survey, one of the main sources of data used to measure migration flows, has been suspended due to the pandemic. Changes in data collection methods may disproportionately affect migrants in the future.

Boys showing their scars, Victoria Square, Athens, Greece. Credit: Karol Grygoruk/RATS Agency. During lockdowns of refugee camps and in arrival countries, schools and language courses were stopped. For many, education continued through online learning, but this is impossible to access for those who do not have internet or necessary digital equipment. In some cases, children who stopped going to school turned to child labour.

Boys showing their scars, Victoria Square, Athens, Greece. Credit: Karol Grygoruk/RATS Agency. The same goes for an even more important witness of the situation: the media. Throughout the pandemic, freedom of the press has been limited, with journalists struggling to access refugee camps in Greece, Serbia, Bosnia and Germany.

Interviewing refugees through fences of Diavata refugee camp, Greece. Credit: Karol Grygoruk/RATS Agency. With new procedures and local laws, the authorities have also tried to silence the refugees inside and outside of the camps, forbidding them to report on their situation or to talk with the journalists. This is in part thanks to a new law in Greece.

Train station Doirani, at the Greek/Macedonian border. Credit: Karol Grygoruk/RATS Agency. Due to less NGOs working locally, as well as fewer journalists covering stories from the borders, pushbacks on the waters and borders are less documented. Justified by the excuse that preventing movement helps reduce the spread of Covid-19, the wider public has been more accepting of pushbacks. Yet very few members of the general public in these countries are aware of the violence and mistreatment of refugees, including women and children, these incidents involve.

Bullets found on the Greek/Macedonian border. Credit: Karol Grygoruk/RATS Agency. For those who, despite restrictions, wanted to help the refugees, new laws were waiting. Restricting and criminalizing NGOs and activists is a weekly occurrence in Greece, Bosnia, Croatia, Italy and France.

Remains of evicted settlement, out of Dunkirk, France. Credit: Karol Grygoruk/RATS Agency. Throughout the pandemic, refugees across Europe have had limited access to information due to language and cultural barriers. Sharing any information regarding Covid-19 is an additional challenge.

Announcement in Ritsona refugee camp, Greece. Credit: Karol Grygoruk/RATS Agency. Refugees, besides having less access to health care, at the same time are unable to socially distance and access water, sanitation and hygiene facilities. Throughout the pandemic, they also struggled to secure Covid-19 testing, since in most countries even basic emergency healthcare may be limited without registration documents. There is also the issue of mental health services and counselling, something that isolated refugees need more than ever.

Muhammad in Diavata refugee camp, Greece. Credit: Karol Grygoruk/RATS Agency. Refugees on the move tend to avoid Covid-19 testing or meeting doctors because of a fear of deportation. This is a valid concern, but is used as a reason by governments to enforce lockdowns. Interestingly, even while most borders were at some point closed in 2020, deportations still continued. In Poland, between 15 March and 20 April 2020 alone, when borders were officially closed, 55 people were deported to Russia.

Anti-deportations protests at Las Raices refugee camp, Tenerife, Canary Islands. Credit: Karol Grygoruk/RATS Agency. For people on the move, lockdowns in countries and cities on their route meant not only empty streets and greater visibility as a result, but also fewer people to offer food, water and other forms of support. With the closure of restaurants and bars, they had no place to stay warm or charge their phones.

Vietnamese settlement close to Grande-Synthe, close to Dunkirk, France. Credit: Karol Grygoruk/RATS Agency. With livelihoods at a standstill and strict quarantines in place, Covid-19 led to a 40 per cent spike in the number of people in need of humanitarian aid. But traditional donor countries and societies, who are facing their own pandemic crises, are instead focusing on domestic relief packages. As a result, there are less resources and political will for foreign aid.

In the centre of Calais, France. Credit: Karol Grygoruk/RATS Agency. Refugees and migrants were often the first to be fired when an employer faced financial troubles during the pandemic. Many registered and unregistered workers in Germany lost their source of income and rights to social benefits.

St. John the Baptist Church at the Béguinage church in Brussels, Belgium, where since 23 January 2021 protests have been taking place. Credit: Karol Grygoruk/RATS Agency. On the top of it all, the rise of xenophobia has become increasingly visible. Some countries even used it as a political strategy: for example, Serbia based their political campaign on anti-migration slogans incited by narratives framing migrants as ‘spreaders’ of the virus.

An area in Las Palmas where the first refugee died at night, because of not being treated in a respectful way, Grand Canaria, Canary Islands. Credit: Karol Grygoruk/RATS Agency. -
By Anna Alboth
‘Maybe you can work remotely during Covid-19, but in my country, already before the pandemic, half of the population was jobless’, says Adama, a 25-year-old man from Senegal. He arrived in Tenerife, one of the Canary Islands, on a boat carrying 50 people from Saint Louis just five months ago. ‘Isn’t it ironic that the big boats stealing fish from our waters, not leaving anything for us, are from the European countries that do not give us Senegalese legal visas or even seasonal work?’
Adama chose the boat because he had no other possibilities. ‘I was sending letters and applications to different countries. I tried to register for schools and aid programmes. I thought I would be someone who can manage, who doesn’t need to come to Europe. But look around: now there are here not only fishermen who lost their fish because of European and Chinese business in Senegal, but also taxi drivers, hotel owners and businessmen whose businesses collapsed in 2020.’
Many people in the same situation as Adama are now travelling to the Canary Islands from Senegal or Gambia, along what is known as the West African migratory route. We have all read about the Central Mediterranean route running from Libya to Malta or Italy. We have all seen hundreds, even thousands, of pictures of refugees following the Eastern Mediterranean route from Turkey to Greece. But how many people are aware that in 2020 more than 23,000 people arrived in the Canary Islands?
Before, refugees would typically try to cross from the north of Morocco through the Spanish enclaves of Melilla or Ceuta. But since the European Union (EU) paid €175 million to Morocco in return for ‘improved migration management’, border control has been strengthened and migration paths have changed in response. While ongoing local conflicts such as those in Mali or Congo, as well as drought in Morocco, have contributed to this shift, the pandemic has also been an important driver. Indeed, Covid-19 has not only influenced many people in their decision to take the West African route, but has also led smugglers to change their usual paths in response to local lockdowns. The Mixed Migration Centre ran a series of surveys among migrants in different regions from the beginning of the pandemic until the end of 2020. In its final global survey, published in December 2020, it noted that the economic fallout of Covid-19 had been a factor in deciding to leave for 30 per cent of the West African migrants surveyed in the region. In one of the mid-year reports, nearly 70 per cent of West African migrants noted that the pandemic had made it harder to cross borders.
To better understand the scale of the challenges involved in the West African route, a quick look at a map is needed. In a straight line, at their closest point, there is 100 kilometres of ocean between Morocco and Fuerteventura, one of the islands. By way of comparison: those making the hazardous trip between Turkey and Greece travel between 12 and 15 kilometres at sea. Most of those travelling the West African route begin their journey in Dakhla, which lies 400 kilometres south of the Canary Islands along the coast of Western Sahara. However, during 2020 other routes became increasingly popular despite the even greater risks involved: from Mauritania, Senegal, Ghana or even Guinea, almost 2,500 kilometres away.
The boat trips that the refugees take involve sometimes as much as 12 days out on the open waters of the Atlantic Ocean. Twelve days without sun protection, in soaked clothes, in the wind.
The boat trips that the refugees take involve sometimes as much as 12 days out on the open waters of the Atlantic Ocean. Twelve days without sun protection, in soaked clothes, in the wind. Twelve days of burns and abrasions. Twelve days of hunger, because smugglers on the African side provide only enough water or rice for the first few days. Sometimes motors break down, the fuel runs out or cookers explode. Sometimes the weather is favourable. Other times the wind can carry the boats far out into the Atlantic, and then there is no rescue. More often than not, the passengers suffer from seasickness and saltwater poisoning, exhaustion and trauma. And though the cost of boarding a boat is prohibitive, with a seat now costing anywhere between €1,500 and €4,000, there is no certainty that the boat will reach its destination: right now, one in five boats is sinking.
While in 2020 this route was mainly used by men, by the spring of 2021 nearly a third of those who arrived were women and children. The refugees arrive in boats called cayucos or pateras. Not a day goes by without such a boat reaching one of the Canary Islands. Some carry 50 people, others 100, in some the number of passengers exceeds 150. After reaching the shore, many people simply ask: ‘Am I in Spain?’
It is worth taking another look at a map: the Canary Islands are 1,700 kilometres away from mainland Spain.
Most Spaniards living on the Canary Islands earn their living from tourism, running hotels, restaurants and water sports schools. The impact of Covid-19 on them has been harsh: for many months the hotels have stood empty and the tourism businesses have collapsed one by one. But now, with flights resuming and Europeans again arriving on Tenerife’s beaches, the possibility of encountering a boat carrying dozens of exhausted refugees has scared away many potential holidaymakers.
Towards the end of 2020, Spain decided to try a new approach that had the potential to shelter its growing refugee and migrant population while also providing a lifeline to its embattled tourism industry. Since the hotels on the islands were empty and there was nowhere to put the arriving refugees, the solution was obvious. Receiving government subsidies, 17 hotels, tourism complexes and holiday resorts have accepted thousands of people in need.
It appeared to be a win-win solution, but some thought otherwise. ‘Migrants on hotel balconies’, grumbled headlines. Some local residents, whose businesses were failing due to the pandemic, voiced resentment at these new arrangements. It was then that the first racist attacks, harassment and beatings began. Since then, with the construction of a number of newly built refugee camps in military barracks in Tenerife, Grand Canaria and Fuerteventura, refugees and migrants have been transferred from the hotels into these cramped, poorly serviced settlements.
One example is Las Raices in Tenerife. There are already about 2,000 people in the camp, divided into 64-person tents. There is hardly any hot water, no regular clothes supply, and people stand in lines for hours. Food is scarce, and more than a dozen people have already ended up in hospital due to poisoning. There is no doctor in the camp at night, and – as in any place where crowds of desperate people from different countries and cultures are forcibly confined in overcrowded, inhumane conditions – conflict can occur. ‘It’s no coincidence that the camp is off the beaten track’, says Roberto Mesa, one of the leading camp activists. ‘Here and all over Europe, refugees are being hidden, cut off from reality, taken out of sight.’
Leaving refugees in the middle of nowhere is just one of the many sins Spanish authorities have committed. For many months they were separating children from their parents on arrival and preventing people on the Canary Islands from crossing to the mainland. People live in fear of deportation and do not get enough information about changes in the asylum process brought on by the pandemic.
A longer analysis of how the pandemic has placed increasing pressures on refugees and migrants across Europe through heightened border restrictions, suspension of asylum processing, discriminatory restrictions and other measures is available here.
Photo: Boys from Mali watching surfers in Puerto de la Cruz, Tenerife. Since many refugees arrived at the Canary Islands this year and most of services and NGOs are not working due to Covid-19, boys spend hours looking into the waves. Credit: Karol Grygoruk/RATS agency.
-
By Emily Bauman
Despite the best efforts of humanitarian actors in Sudan, refugees, migrants and other displaced people in the country are struggling amidst the dual effects of the coronavirus and renewed violence. For the 1 million displaced by armed violence in the Tigray region of Ethiopia, the pandemic is making it even harder to find a safe haven within an insecure, resource-scarce landscape.
A significant number of these are now seeking sanctuary in Sudan: according to UN High Commissioner for Refugees (UNHCR), by the end of April 2021 more than 63,000 Ethiopians had crossed into Sudan since the outbreak of civil conflict in November 2020.
In addition to the new Ethiopian arrivals from Tigray, the context of forced displacement and Covid-19 in Sudan also features the ongoing crisis in Darfur and urban refugee populations in major cities. According to data published by the International Organization for Migration (IOM), which is providing humanitarian assistance in the region, in less than four months of 2021 close to 237,000 people were displaced by conflict in Darfur – more than four times the number (53,000) who were displaced by conflict during the whole of 2020. In a world of limited capacity, partners and resources that would otherwise be available to assist with the more general humanitarian response are instead focusing their efforts on Covid-19 emergency programming.
For example, of the 250,000 internally displaced people (IDPs) in Darfur in need of health care services, only about 65,000 people were able to access them as of May 2021. General practitioners and many hospitals are dedicated exclusively to managing Covid-19 cases, leaving other life-threatening conditions largely untreated. For pregnant refugee and displaced women in Darfur and elsewhere in Sudan, this often means that pre-natal check-ups or skilled care during and after deliveries are simply unavailable. Meanwhile, amidst the oncoming third wave of the pandemic in Sudan, the security situation in Ag Geneina town, Darfur, is tense and unpredictable. The situation in gathering sites in Ag Geneina is critical because of insecurity due to armed clashes, and overcrowding and unsanitary conditions which further raise infection rates. Unsurprisingly, Sudan’s already weak health care system has been struggling to respond to the Covid-19 outbreak, especially in its conflict-affected regions.
The pandemic has also put pressure on already strained inter-communal relations. Refugees arriving in Sudan from Tigray and IDPs in Darfur often seek refuge in sites near communities which are dealing with their own struggles, such as limited access to water and increasing tensions over shrinking grazing areas for their cattle herds: the friction between these host communities and those living in the camps or informal sites has worsened in the wake of Covid-19. The risk of potential unrest is now elevated by rising anxiety among host communities that the incoming refugees and displaced are bringing the virus to their doors.
The Food and Agriculture Organization (FAO) estimates 7.1 million people are severely food insecure in Sudan, including about 2.5 million internally displaced persons and 1.1 million refugees.
Pre-existing causes of instability and vulnerability, namely the lack of services, unemployment, environmental degradation, economic crisis and inadequate government investment have been accentuated by the influx of potentially Covid-infected Ethiopian refugees to eastern Sudan. Because of the cultural and ethnic differences between the two groups and pre-existing conditions, there is a risk that long-standing causes of instability are by proxy attributed to the influx of refugees by the host community. For example, tensions over fears of disease outbreaks or environmental degradation (such as cutting of trees for firewood) have already been reported, further driving negative perceptions of refugees by the local communities. As a result, humanitarian agencies must redouble their efforts to raise funding and execute communication campaigns that foster peace, mitigate inter-communal tensions and spread correct information about Covid-19, while also creating projects that directly address the socio-economic impacts of refugees during a pandemic.
For urban-based refugees, migrants and IDPs in Sudan, the lockdown measures imposed in response to the pandemic created a lack of mobility that brought work in the informal economy to a standstill. Given that many urban refugee and displaced households rely on small informal jobs for their day-to-day survival, food insecurity for these and other migrant communities in Sudan soared from the onset of the pandemic. In a city like Khartoum, the inability to work in informal economy jobs due to Covid-19-related lockdowns placed hundreds of thousands of refugee, internally displaced and migrant households at risk of starvation in 2020. According to the latest estimates from the Food and Agriculture Organization (FAO), overall about 7.1 million people are severely food insecure in Sudan, with some 2.5 million internally displaced people (IDPs) and 1.1 million refugees, mainly from South Sudan and Ethiopia, facing substantial humanitarian needs.
Organizations like IOM are evolving quickly to meet the additional complex needs of refugees and displaced people fleeing violence amidst the virus. Multiple creative solutions are being used to overcome the compounded challenges, and social cohesion programmes are more vital than ever. The support and interventions of the international community are pivotal to alleviate the pressure of refugee and IDP influxes on host communities and increased tensions due to perceived spread of the pandemic by refugees, and to enhance their inclusion and participation in the socio-economic recovery of the localities where they live. Promoting solidarity and defusing possible future tensions over limited basic services, natural resources, health and infrastructure remain imperative, while also continuing to support refugees and displaced people with critical services.
Awareness-raising campaigns in camps, settlements and cities about preventing the spread of Covid-19 have become a core part of the work for the Sudanese government, humanitarian agencies and their partners. This has become an important element of information and training sessions that were previously focused on issues such as human trafficking and migrant rights. Humanitarian agencies have switched from in-person to virtual meetings, and to bilateral instead of round-table formats for coordination meetings where possible. Land lines and cell phones have come back into play. In remote areas like Darfur, where internet-based calls are not possible, emergency assistance teams resort to telephone calls for information sharing with migrants and to offer services like psychosocial support or coordinating assisted voluntary return to the migrants’ home countries. Hotlines for Covid-19 assistance and essential services are being set up across Sudan.
Providing support to refugee and displaced leaders, as well as migrant community focal points, has been recognized as more essential than ever to meet the unprecedented challenges of responding to crisis situations during a global pandemic. IOM trains community leaders in Sudan to identify cases in need of protection amidst their constituents, to help spread awareness about Covid-19 prevention, further disseminate information, provide referrals to hospitals and other services, and identify those most at risk, including the most food insecure, for emergency intervention.
While creative solutions are being found, the impact of the coronavirus is creating a silent yet unprecedented challenge to humanitarian operations. Aid workers – often specialists who are difficult to replace quickly – are also contracting the virus in the field and becoming incapacitated for weeks or months at a time. So when an emergency response operation in remote areas of Sudan hinges on the expertise, community relationships and health of a few people, usually working around the clock, but who are then themselves infected and out of commission, it affects the lives of hundreds, often thousands, of refugees, IDPs and host community members. This is particularly critical in settings where multiple overlaying emergencies are ongoing at once, such as famine and historic levels of flooding that have further jeopardized the health and security of tens of thousands of people.
In the context of the Tigray crisis and Darfur, there is currently a race against time. The international aid effort requires adequate staffing and urgent coordination, with over a dozen agencies currently building thousands of latrines and shelters, as well as helping to construct roads before the rainy season brings floods and makes access to the refugee and displaced sites impossible. Whether this daunting feat will be possible amidst the myriad factors of the emergency response and the added complexity of the coronavirus remains to be seen.
Photo: Ethiopians who have just crossed a river from Ethiopia to Sudan to flee from the Tigray region, walk towards the Hamdeyat refugees transit camp, which houses refugees fleeing the fighting, on the border in Sudan, December 1, 2020. Credit: REUTERS/Baz Ratner.
Identity and well-being
Embrace holistic, locally appropriate pandemic responses that recognize and respect community perspectives, practices and beliefs: Public health strategies should be adapted to the particular contexts of minorities and indigenous peoples to ensure their effectiveness while protecting cultural knowledge, traditional lifestyles and mental health. The imposition of standardized measures such as lockdowns and border closures has been justified by the need for equitable and coherent public health strategies. Yet in practice, for minorities and indigenous peoples, the impacts of these measures have often been felt unevenly and included many unseen costs to social cohesion, identity and mental health. When imposed without consultation with marginalized communities, the unintended consequences of impractical regulations (such as restricted movement on nomadic populations) can leave lasting damage to social and economic well-being. On the other hand, when policies are participatory and aligned with the needs and values of these groups, their effectiveness will be greatly improved while the social and psychological burdens are reduced.
- 01

Guatemala: A lifeline for survivors of gender-based violence during lockdown
By Laura Quintana Soms Gender-based violence, particularly against indigenous women and girls, is entrenched in Guatemala. The country’s long-standing problem of femicide – often described by activists as an ‘epidemic’ – has…
0 min read
- 02

Pacific: Containing Covid-19 through cultural practices and a rights-based approach
By Joshua Cooper In the early months of the pandemic, as countries across the world contended with the ravages of a new and unpredictable virus, the Pacific offered a rare success story. While much of the world took a wait-and-see approach…
1 min read
- 03

Sweden: For Sámi communities, Covid-19 border controls could threaten a way of life
By Oula-Antti Labba Nils Vasara-Hammare, a Sámi reindeer herder, environmentalist and school principal, has spent all of his life in the traditional territory of Sámiland (Sápmi) on the Swedish side. Until recently, he rarely had to…
1 min read
-
By Laura Quintana Soms
Gender-based violence, particularly against indigenous women and girls, is entrenched in Guatemala. The country’s long-standing problem of femicide – often described by activists as an ‘epidemic’ – has been aggravated by the outbreak of Covid-19.
Between March and June 2020, during lockdown, at least 140 women were murdered, 57 of whom were classified as victims of femicide by the Prosecutor’s Office, while authorities received more than 19,000 reports of violence against women. During this same period, 403 emergency alerts were issued to track down women who had disappeared, including the first alert ever activated for a trans woman in the country, La China.
The pandemic has also had a deep impact on local and national non-governmental organizations which, already operating in extremely stressful and dangerous circumstances, have had to adapt their activities to the new context almost overnight. This was the case for Casa Aq’ab’al, a local organization based in the village of San Lucas Tolimán, where the population is largely Maya Kaqchikel. Created in 2016 with the objective of supporting survivors of domestic violence after the murder of a 16-year-old girl, Casa Aq’ab’al supported over 60 survivors of gender-based violence and their families between July and December 2019. The organization had planned to maintain this level of support during 2020, but when Covid-19 reached the village its five staff members suddenly found their work dramatically curtailed. They realized that they needed to respond quickly to this new challenge to ensure the right of indigenous women and girls to live without violence was protected.
First, there was the problem of increased isolation, as vulnerable women and girls were suddenly cut off from external sources of support. Like other countries, Guatemala applied a strict lockdown from March 2020, with long curfews and stay-at-home restrictions that increased tensions at home while making it impossible for women to report violence and reach out for help. Authorities tried to address this issue by implementing new or improved reporting systems, such as emergency hotlines and the creation of a mobile phone application as a ‘panic button’ for women to ask for help. Yet, with less than half of the population regularly using the internet, and an even smaller proportion having access to a secure connection at home, these options are not available to many of those at risk.
Casa Aq’ab’al distributed milk, vegetables and other items to more than 200 people, with over 90 per cent being women survivors of domestic violence and their families, the majority with precarious incomes.
At the same time, the Covid-19 crisis has placed further strain on an already overburdened and poorly functioning judicial system for reporting and investigating incidents of violence against women. As a result, many hearings and investigations have been delayed or suspended: during lockdown, Casa Aq’ab’al was only able to resolve one legal case while over 30 others were pending. More recently, the law courts have begun moving forward, with the resolution of new cases and the review of pending ones. Nevertheless, the underlying weaknesses of the country’s judicial system remain: Guatemala still ranks 118th out of 128 countries in the World Justice Project’s global ranking.
In parallel to these institutional pressures, Casa Aq’ab’al also faced the issue of their beneficiaries and neighbours suddenly losing their income. In a village where most people live from day to day, not being able to go out and sell food, clothes and other products to locals and tourists left many families in a dire economic situation. In a country where almost half the population was already unable to afford the basic food basket and levels of childhood stunting are among the highest in the world, the health implications for the most marginalized communities are potentially devastating — even before the risk of the virus itself is also factored in.
Although Casa Aq’ab’al decided to close during the first weeks of the pandemic, the team immediately reviewed the changing needs of their beneficiaries and the projects which were to be implemented during that period. Thanks to the flexibility of their donors, they were able to rearrange priorities and open up new directions for action. One critical focus area was food. With this in mind, staff created a database of families with low or insecure incomes and distributed — in collaboration with other organizations, a hotel and local volunteer firefighters — emergency supplies to those most in need. To avoid duplication, those families on Casa Aq’ab’al’s database were also incorporated into the priority lists of the local authorities in order to ensure support was maintained sustainably and that households in the most extreme situations were prioritized. In total, Casa Aq’ab’al distributed milk, vegetables and other items to more than 200 people, with over 90 per cent being women survivors of domestic violence and their families, the majority with precarious incomes.
Following this immediate response, the team decided to start installing home and community gardens for survivors of domestic violence, mainly adult women, to grow their own vegetables and herbs. In this way, food provision in the medium term would no longer be an issue. The project was also designed to support the revival of creole and organic seeds, instead of using transgenic and imported seeds. Casa Aq’ab’al now has four community allotments and more than 30 family gardens. The benefits extend beyond nutrition, providing a vital shared social space where women can meet and share their gardening experiences when they see each other in the market or in the streets of the village — bringing an end to the long years of isolation they have frequently experienced as survivors of domestic violence. In the community gardens, women coordinate among themselves the planting and maintenance, and share their experience and knowledge of caring for plants and vegetables with their families.
In parallel, the team organized workshops for women survivors of domestic violence on the production of organic soap, solid shampoo and other health and beauty products from plants grown in the organization’s gardens, such as rosemary and lavender, building on ancestral knowledge of the lunar cycles and the Mayan spiritual calendars. This led to the creation of a brand which is now sold within Guatemala, providing a number of women survivors of domestic violence with a sustainable income.
Photo: A group of women survivors of gender-based violence engage in a talk with Casa Aq’ab’al’s psychologist on the history and importance of 8 March (Women’s day). Credit: Casa Aq’ab’al.
-
By Joshua Cooper
In the early months of the pandemic, as countries across the world contended with the ravages of a new and unpredictable virus, the Pacific offered a rare success story. While much of the world took a wait-and-see approach to the pandemic, not wanting to halt the global economic engine, governments in the Pacific acted swiftly with proactive policies to save their populations from the pandemic.
Six months after it began, there were just 10 countries (excluding two dictatorships whose claims to be Covid-free were not credible) that had yet to experience a single reported case of the virus – and all of them were in the Pacific.
While some of the world’s richest countries suffered unimaginable upheaval, with mounting deaths and full lockdowns, the Pacific Islands focused on sustainable practices rooted in ancestral wisdom and traditional livelihoods, drawing on their cultural knowledge to counter the pandemic. Oceania had lessons from previous health crises and was determined to be decisive to save lives. This approach encouraged a proactive, preventive policy approach to Covid-19 that kept communities sealed off from the spread of the virus.
Aotearoa (New Zealand) has, throughout the pandemic, been spared major outbreaks of the virus due in part to its strong precautionary approach through strict enforcement of measures such as quarantine to prevent widespread transmission. Borders were also closed to international travel as Prime Minister Jacinda Ardern, noting the country’s role as a key departure hub, took responsibility to protect its Pacific neighbours through early action. By the end of April 2020, Aotearoa concluded five weeks of strict level-four lockdown, with three-quarters of the country’s economy returning to operation.
Aotearoa was also one of the first nations to successfully eliminate Covid-19 from its country. Female leadership has generated growing support for a holistic strategy to manage the pandemic, but Ardern has also acknowledged the important role of Māori ancestral wisdom in guiding not only the government but also grassroots action. A key element in this was manaakitanga, a central concept of the Māori worldview honouring connections among communities and an obligation to organize beyond one’s own good. At its core, manaakitanga maintains that other members of one’s community have importance equal to, and even greater, than one’s own. Its principles are not only an ancestral pillar in the cosmology of the host culture, but also widely known among the general population as they are now taught in Aotearoa schools.
Elsewhere in the Pacific, prompt and decisive efforts rooted in education were also essential in preventing the spread of Covid-19. Following a successful information campaign in the initial stages of the pandemic that focused on the science around the virus and the necessary steps to protect against it, August 2020 saw the launch of a unique United Nations (UN) initiative, ‘Pacific Unite: Saving Lives Together’, partnering with Pacific Islands advocates, activists, athletes and artists. This was a first-of-its-kind televised and digitally streamed concert rippling across Oceania, strengthening the human rights and public health movement around containing the pandemic in the Pacific.
The virtual concert was hosted by Aunty Tala from the Laughing Samoans, featuring messages delivered by high-level advocates from the UN, heads of state of Pacific Island countries, celebrities and artists, including music with a message from Te Vaka and Poly Flavour. All entertained while educating audiences about the best ways to continue the positive public policies of prevention and protection of all Pacific islanders. The Pacific Unite concert was the first-ever virtual concert by artists from Oceania that was accessible to all audiences across the Pacific Islands and around the planet, highlighting the strength of a rights-based approach to managing the pandemic and honouring the contribution of essential workers to the fight against Covid-19. It was also a call to remain vigilant, as the threat for many vulnerable communities in the Pacific still remained.
The quick action to close borders in the Pacific was also rooted in an awareness that, if the virus did spread, it could prove disastrous in many states where health facilities were chronically under-resourced and unable to cope with a crisis of this magnitude. In the Solomon Islands and Nauru, for instance, there were no intensive-care unit beds available and the Cook Islands had just two respirators.
Tragically, 2021 has been a brutal reminder of Covid-19’s capacity to surge rapidly from a handful of cases, even in areas previously spared from the worst of its impacts. At the beginning of March 2021, while the nation mourned the passing of founding father Michael Somare and the pandemic had just entered its second year, Papua New Guinea faced a sharp rise in infections as the virus spread to 19 of the country’s 22 provinces. With limited testing capacity, it is likely that only a fraction of infections were traced. In a context where the health infrastructure is already understaffed, the country’s public health system could face collapse without effective action. The knock-on effects for other areas of health – for example, in curtailed gynaecological and natal care for women and girls – have already been felt.
While a vaccination programme prioritizing frontline health workers was initiated in Papua New Guinea in May 2021, other countries such as Fiji have had to implement drastic measures to contain the virus. The Fiji authorities closed the second-largest hospital and quarantined hundreds of patients and staff after a patient who later died was found to have infected a doctor. It is to be hoped that the prudent policies that have spared Pacific populations during the first year of the pandemic will continue to prevent the spread of the virus. Given the poor state of infrastructure and services across the region, however, the Pacific governments must prepare for worst-case possibilities. In this scenario, it is vital that other countries – who learnt so much from the positive practices of the Pacific and now, after a year of battling the virus, have lessons of their own to share – provide adequate assistance to Oceania should it be needed.
Photo: Scenes from the ‘Pacific Unite: Saving Lives Together’ concert, televised and digitally streamed across Oceania. Source: ABC iview.
-
By Oula-Antti Labba
Nils Vasara-Hammare, a Sámi reindeer herder, environmentalist and school principal, has spent all of his life in the traditional territory of Sámiland (Sápmi) on the Swedish side. Until recently, he rarely had to worry about the national borders that have divided Sápmi into four parts.
Before the pandemic, he did not even need to bring his passport when crossing the border from Finland or Norway: normally, citizens of one of the Nordic countries can cross into a neighbouring country freely. Therefore, it is only natural that Sámi living in this area say that they are going to ‘the Norwegian side’ or ‘the Finnish side’, not Norway or Finland. ‘We Sámi think that we are in Sámiland when we cross the border,’ explains Vasara-Hammare. ‘In a normal situation, when we drive on the road on the Finnish side, it doesn’t feel as if we are in another country.’
With the outbreak of Covid-19, however, everything changed. ‘This year we have also realized how dependent we are on the Finnish side in many ways.’ In the wake of the pandemic, border restrictions have been tightened across Sápmi, dividing Sámi families and communities residing across the state borders of Russia, Finland, Norway and Sweden. These have had a significant negative impact on traditional Sámi reindeer husbandry, especially the cross-border reindeer-herding work of the Sámi people.
For the Könkämä Sámi reindeer-herding community on the Swedish side of Sápmi, who are dependent on areas inside the borders of three nation states, the restrictions have brought major disruption to the everyday life of the community. While the community’s winter, autumn and spring pastures are on the Swedish side of Sápmi, their summer pastures are on the Norwegian side of the territory. At the same time, to reach their reindeer pastures and herding bases, they have to cross to the Finnish side in order to use the only south-to-north main road in the area.
‘The road on the Finnish side is very important to us. When Finland closed the borders, then the authorities insisted that we choose specific members of our Sámi community to cross the border. It was an unfortunate situation that I was forced to tell most of the members that you cannot cross the border in order to practise your traditional livelihood,’ says Vasara-Hammare. Border control by the Finnish authorities at the Gárasavvon check point, on the border with Sweden, became much stricter than before. Officials there generally did not appreciate the specific situation of the Könkämä Sámi community and lacked knowledge about the Sámi region more broadly.
As a result, community members were severely affected by this sudden securitization. Signs on the border of Sweden and Finland read: ‘Crossing the border outside the border checkpoint without a permit is a state crime.’ This distressed many Sámi and left them feeling almost like criminals when moving through their traditional lands, just as their ancestors have done since time immemorial. ‘There was a decision that we could cross the border only at five different locations,’ says Vasara-Hammare. ‘There was also a camera and border control on the bridge that we crossed on our way to our annual reindeer calf markings in Geaidnovuohpi, even if we had gone through border control in Gárasavvon. I thought that that was unnecessary – we were on our traditional lands.’
Borders came to Sápmi, which is located in the northern part of Scandinavia and across Russia’s Kola peninsula, in the eighteenth century when the division of Sámi territory was brokered between Denmark–Norway (the latter at that time was under Danish rule) and Sweden in 1751. This led to a border agreement which included a protocol (Lappekodisil) that recognized the rights of the Sámi people to move across the state borders with their reindeer. The Napoleonic wars of the early nineteenth century brought drastic changes to the map of Europe, as territories were swapped and borders were redrawn, including the separation of Finland from Sweden in 1809 and its absorption into the Russian empire – in the process transferring most of the Sámi reindeer herders from one sovereignty to another. Subsequent border closures between Finland (still under Russian control at that time) and first Norway and then Sweden had a profound impact on reindeer-herding Sámi. Nevertheless, the 1751 Lappekodisil protocol has never been formally repealed.
Now, in the midst of a pandemic, the legacy of these borders is concretely being felt by Sámi communities whose way of life has been thrown into upheaval. During normal summers, Vasara-Hammare’s Sámi community would cross to their summer pastures on the Norwegian side to herd their reindeer and mark their reindeer calves. During the summer of 2020, however, this was not possible for practical reasons. ‘We could have had access to the Norwegian side, but we would have needed to spend 10 days in quarantine and prove that we had been in quarantine,’ says Vasara-Hammare. In addition, the winter before (2019-20) was extremely harsh for the reindeer due to climate change, with earlier and heavier snowfall, several layers of ice and a later-than-normal melting of the snow. ‘It was a really stressful winter and spring in many ways,’ says Vasara-Hammare.
The border closures and restrictions during the pandemic will have a long-term effect on Sámi traditional livelihoods. Because Sámi traditional livelihoods are important conduits of Sámi language and culture, the restrictions could have far-reaching effects on the community’s way of life. As the Sámi Parliament of Sweden has reported to the United Nations, the pandemic could have potentially devastating impacts on the inter-generational transmission of traditional knowledge in Sámi society.
In December 2020, the Finnish government recognized the rights of the Sámi to cross its borders into Norway and Sweden. The government decided that residents of the border communities and Sámi may cross overland and across lakes and rivers at other places besides the authorized border crossings during the pandemic. However, these rights are based only on the decision of the government and not on a separate, binding act of law.
As a result, the situation is uncertain as to how state borders will in the future interfere with the daily lives and interactions of the Sámi people. ‘Of course,’ says Vasara-Hammare, ‘the fear exists. The pandemic has shown that states can close the borders – even if Nordic cross-border cooperation has been good before.’
Photo: The border between Sweden and Finland. Credit: Oula-Antti Labba.