50 years of Minority Rights Group
The chapters
This collection of essays draws on the many strands that characterize our work across this time period.
- 01

Introduction
The best qualities of humanity have, throughout history, attracted individuals of high calibre to step beyond their comfortable worlds to reach out in support and assistance to others. Their actions, born out of kindness and empathy, and…
0 min read
- 02

David Astor remembered: ‘MRG could not have dreamt up a more perfect champion’
By Shaun Johnson A book on my shelf that I especially treasure is titled David Astor and the Observer (David Astor was Editor of the Observer from 1948 to 1975). In it, the biographer Richard Cockett gives a fine account of the sweeping and…
0 min read
- 03

Reaching the most marginalized: an intersectional approach to minority rights
By Nicole Girard The mandate of MRG has changed and evolved over the past couple of decades as the organization has redefined its approach to minority rights. Consistent throughout these changes, however, is the effort to realize the rights of…
0 min read
- 04

Sri Lanka: using arts and poetry to confront the legacy of conflict for minority women
By Nicole Girard MRG became involved with Tamils in Sri Lanka with our first report in the 1970s, with regular updates thereafter. By the time Neelan Tiruchelvam joined MRG’s International Council in 1994, MRG was establishing a South Asia…
0 min read
- 05

Ensuring accessible education
By Claire Thomas Although human rights in essence date back centuries, if not millennia, human rights as a movement really began to take off in the 1960s and 1970s. MRG’s birth was therefore at a moment when many like-minded groups were…
0 min read
- 06

United Kingdom: The Voices project – a unique platform for refugee children to share their storie
By Rachel Warner Voices was a series of dual-language booklets of autobiographical writing by young asylum seekers and refugees in London schools, published by MRG in the 1990s, to meet a growing need for materials that reflected the…
0 min read
- 07

Addressing health inequalities
From the beginning, MRG has systematically focused on health services and the barriers that minorities and indigenous peoples face in accessing them. The disparities, while often overlooked, are striking: where statistics are available, health…
0 min read
- 08

Kenya: To identify discrimination, we first need to get the data – health inequalities among Somali women in Mandera County, Kenya
By Claire Thomas A recent and ongoing example of MRG’s work on health focuses on minority and indigenous women in Cambodia, Ethiopia, Kenya and Myanmar and their right to equally access sexual and reproductive health services such as…
0 min read
- 09

Making voices heard at the international level
By Neil Clarke MRG’s work with the UN has been one of the cornerstones of its work and identity over the last 50 years. The organization’s profile as the leading international non-governmental organization (NGO) in the field of minority…
0 min read
- 10

Supporting the creation of a new UN minority issues mandate
By Evelin Verhás By the early 2000s, the indigenous peoples’ rights movement had successfully achieved the creation of several UN mechanisms devoted to indigenous issues, including a Working Group, a Permanent Forum and a Special…
0 min read
- 11
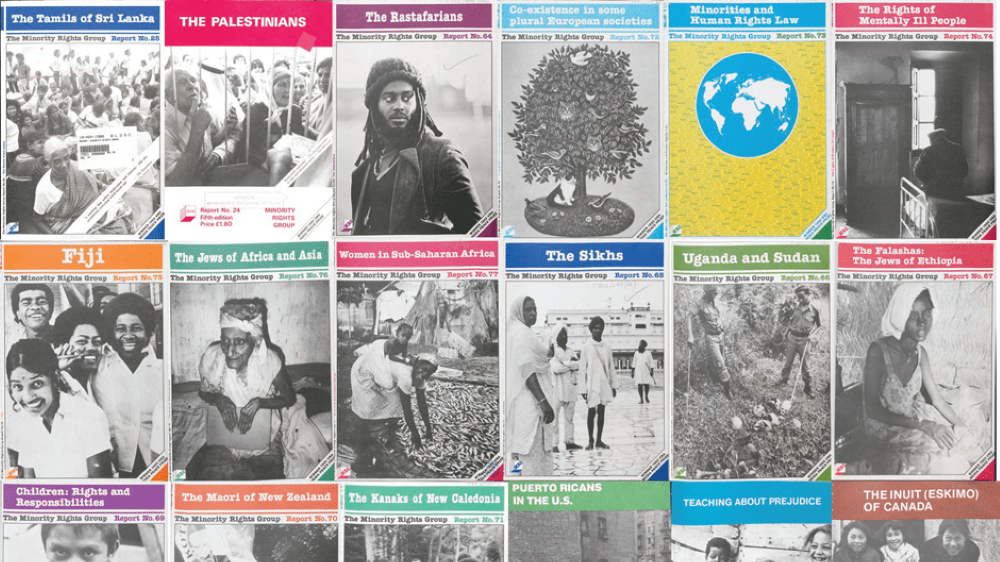
Making minorities and indigenous peoples visible: the role of MRG’s research and publications
By Peter Grant In 1970, shortly after our foundation, MRG launched our first publication: Religious Minorities in the Soviet Union. This was followed shortly after by other reports, ranging from the situation of Aboriginal Australians and that…
1 min read
- 12

The World Directory of Minorities and Indigenous Peoples
By Alan Phillips The year 1989 was a watershed for minority rights in Europe. The tearing down of the Berlin Wall in Germany symbolized the rejection of the Communist system by the people of Central and Eastern Europe. Although MRG was a very…
0 min read
- 13

Challenging colonial legacies: Minorities and indigenous peoples’ struggle for inclusion in Africa
By Hamimu Masudi The dubious origins of statehood in Africa have been clear to anyone interested in understanding and explaining contemporary development challenges on the continent. By the stroke of a pen at a Berlin conference in 1884, the…
0 min read
- 14

Capacity-building for minority and indigenous leadership
By Chris Chapman Providing support to minority and indigenous representatives has always been a central part of the MRG ethos. For many years the organization has been running training workshops for activists, first in Geneva and Strasbourg,…
1 min read
- 15

Mauritania: ‘I saw that the system was unjust – it strengthened my resolve to combat injustice’
By Chris Chapman Salimata Lam has been an activist all of her adult life, since joining a pro-democracy movement in her teens. In the 1980s, she was even deported from the country for three years and stripped of her citizenship, which only made…
1 min read
- 16

Adapting to new crises: Meeting the challenge of Covid-19
By Rasha Al Saba From conflict to climate change, MRG has repeatedly reoriented its work in the face of new crises to ensure that minorities and indigenous peoples – frequently the most affected by these challenges – are not forgotten. Most…
1 min read
- 17

Challenging hate: The struggle for the rights of Roma
By Neil Clarke Numbering at least 10 million, though the actual numbers are likely higher, Roma make up the largest ethnic minority in Europe. Roma populations can be found in every country and, while it would be wrong to perpetuate the image…
0 min read
- 18

Dominican Republic: Using film to tell the story of Dominicans of Haitian descent
By Sofia Olins When I first met Rosa Iris, she was completing her law degree while raising her 6-year-old son alone. This, in the compromised conditions of a bateye (a town of corrugated shacks with no water and electricity), is no easy…
0 min read
- 19

Iraq and Syria: Documenting human rights violations in conflict – the Ceasefire online reporting tool
By Miriam Puttick In conflict zones around the world, violations against minorities are often an inseparable element of the core conflict dynamics. States and armed groups will often harness long-standing tensions and stoke hatred against…
0 min read
- 20

Iraq: ‘We need real and effective political and economic participation – it should not be décor’
By Chris Chapman Mikhael Benjamin is an Assyrian-Christian activist from Iraq who has devoted his life to fighting for the rights of his community, first in a political party, and since 2005 in the human rights movement. Since the beginning…
0 min read
- 21

Kenya: ‘The Ogiek journey in the corridors of justice, from Kenya to Banjul then Arusha, was never a bed of roses, it had ups and downs, but thanks to MRG’s support throughout, the litigation process was a success’
By Lucy Claridge In 2017, the African Court on Human and Peoples’ Rights issued its first ever ruling on indigenous rights in a case brought by MRG in partnership with Kenya’s Ogiek community. Numbering around 30,000 people,…
1 min read
- 22

Litigating indigenous land rights: a model for conservation
By Lucy Claridge MRG’s strategic litigation programme was established in 2002, in response to the clear need for specific legal tools to combat violations of the rights of minority and indigenous communities throughout the world. It aims to…
0 min read
- 23

Managing and preventing conflict: a minority rights-based approach
By Chris Chapman From the outset in 1970, MRG reported on many areas of violent conflict where the rights of minorities and indigenous peoples were denied and where others remained silent for fear of being associated with secessionists or…
0 min read
- 24

Pakistan: Pragmatism or idealism? Advocating against blasphemy laws
By MRG’s former Head of Programmes In my time at MRG, we worked on numerous programmes on Freedom of Religion or Belief (FoRB). We advocated for an end to the death penalty for apostasy in Mauritania. In India and Bangladesh, we…
0 min read
- 25

Protecting and promoting the rights of religious minorities: an evolving approach
By Silvia Quattrini Freedom of Religion or Belief (FoRB) is usually defined as the freedom to adopt, change or renounce a religion or belief and it involves principles such as freedom of worship and freedom from coercion. Unnecessary…
0 min read
- 26

The power of innovation to create lasting change
By Claire Thomas MRG is not an organization that has set out to be innovative for its own sake: however, it is an organization that listens hard to the people whose interests it exists to serve. And this commitment to listening to the…
0 min read
- 27

Ukraine: Empowering civil society to turn the tide of anti-Roma hate crime
By Yulian Kondur Hate crime has become an increasingly pressing issue in Ukrainian society, particularly since the beginning of 2018, when the number of attacks on representatives of the Roma community and LGBT+ groups has risen. Violence was…
0 min read
-
The best qualities of humanity have, throughout history, attracted individuals of high calibre to step beyond their comfortable worlds to reach out in support and assistance to others. Their actions, born out of kindness and empathy, and extolled in countless stories and exhorted for centuries by philosophers and faith leaders, led them to stand up for the oppressed, while seeking to amplify their voices and do what they can to safeguard those far from sites of power against their oppressors.
Minority Rights Group International (MRG) owes its existence to this tradition. In the days when David Astor imagined the need for such an organization it was clear that there were people ‘with voice’ and those with none. It was a period of hope, but old fears loomed not far away. Decolonization had freed vast swathes of territories from colonial rule, the devastation of the Second World War was in the rear-view mirror, and fledgling African and Asian states were beginning to take their places on the world stage. However, stories of ethnic violence and unrest were never far from the surface, whether rooted in recent history – the reappearance of anti-Semitic graffiti in European streets, for instance – or new developments, such as the arrival of African and Asian families in search of work whose experiences of stigma and discrimination continue to echo generations later. Giving voice to the voiceless may well have been a theme that motivated and drove our predecessors at MRG, sustained by a belief that research, insight and reason would enable conversations about truth to power that would ultimately prompt lasting change. Written into this was the assumption of the good in the human spirit: that empathy with humanity would win the day.
It is beyond any doubt that MRG was born of privilege. Its early pace-setters chose to use that privilege as a platform to argue, reason and negotiate with those in power with the specific purpose of achieving significant administrative, legislative and judicial changes that would ensure the realization of the inherent dignity and worth of every individual from a minority or indigenous background. Located in London, the capital city of one of the modern world’s most notorious colonial powers, the United Kingdom, it sought to use its place at the table to argue for those not invited to attend.
Fifty years is a very long time for an organization of the size and complexity of MRG. This collection of essays draws on the many strands that characterize our work across this time period, written by some of the incredible people who worked and continue to work for us. In the initial phases much of this work probably sought to ‘give voice to the voiceless’. Looking back at our earliest reports, it is clear that our predecessors drew attention to minorities and indigenous peoples whose issues had not received much, if any, world attention. The impact this had – the simple act of public recognition for communities who were sometimes not even officially acknowledged by their own governments – should not be underestimated: time and again, we hear from now elderly minority and indigenous activists who contact us to say that an early MRG report was instrumental in their own rights awareness.

Two Lisu girls in Shan State, Myanmar / Jenny Matthews/Alamy. But the more we have listened, learnt from and grown in our admiration of the communities we partner and struggle with, the more we have realized our own implication in a deeply unjust international society and sought to, instead, refocus our efforts on disrupting, fixing and reconstructing sound systems to tune out the ambient noise that continues to silence the voices of minority and indigenous communities. This requires, of course, the courage not only to call out the abuses of governments, corporations and armed groups, but to also reflect on our own positionality in the power structures that serve to exclude and marginalize these groups.
Minority rights is one of the oldest antecedents to the development of the Law of Nations. Its prevalence in the earliest treaties and agreements signed between states was far greater than principles of human rights law. Yet power and privilege over centuries ensured that it stayed in the margins, called on at key moments to present a civilizing hue to naked quests for power and domination that sought to subjugate all who presented themselves as obstacles. Minorities and indigenous peoples never self-defined themselves that way, nor specifically sought to stand in anyone else’s way. We merely became ‘minorities’ and ‘indigenous peoples’ as others sought to harness what we had and sought to rally their greater numbers in a bid to revoke rights through the exercise of force and subterfuge.
The human rights framework that emerged most strongly with the creation of the United Nations (UN) appeared to have finally found a way to guarantee the rights of all. In the centuries-old legal battle between Order and Justice, almost always won by Order even when it meant imposing an unjust order, it instead emphasized the notion of Justice. However, at its very foundations the minority experience was relegated from the human rights headlines, despite the specific experience of Jews and others as minorities targeted by genocidal actions, that led to the key moments in the founding of the organization. The task adopted then, especially relevant in today’s troubled times, was that rather than emphasizing that minorities’ lives matter, it was important instead to guarantee that all lives mattered. The key difference, then as now, is that one calls for structural change, the other is merely a statement of an obvious value.
For indigenous peoples, a different equally promising dawn appeared. High on the UN priority list was the celebration of the notion of self-determination, accompanied by stirring words against oppressive colonial rule. In many cases, however, the processes that flowed from this principle merely transferred power from white colonial rulers to men from dominant ethnic, religious or linguistic communities, often aligned closely with power and speaking its language, to start a reign of a different hue.
So here we stand – more than 50 years later in 2020, in the midst of a pandemic that has disproportionately affected minorities and indigenous peoples. The failure to create inclusive societies has simply meant that ever more mediocre men from dominant majorities can ascend to power. Hate has been decimating our societies, dividing us into narrow vote banks, fostering artificial ‘majorities’ as desperate despots keen to seize levers of power, with neither the vision nor the solutions to societies’ many problems, utilize the obvious: large numbers trump small numbers.
The quest for democratic governance has turned into a simple game of numbers far removed from the hallowed values that underpinned its birth. The generation of these is achieved through complicated algorithms that use personal identity data available to a select group of corporations. This facilitates the construction of complex formulas to ensure that scapegoating of opponents can, through a calculated reach that includes a toxic mix of hate speech, fake news and intimidation, result in influencing individual voter decisions. These mechanisms disseminated en masse, targeted to an angry disenfranchised public faced with a sense of crisis and the drying up of economic opportunity, has created our distasteful dissonant present. The state of disrepair in public life, especially the conspicuous lack of governance abilities among many of those supposedly responsible for governing, has been deeply exposed by the recent outbreak of the pandemic. Global society today has effectively reached a fork in the road.
The perpetrators of hate politics who drive narrow conceptions of identity to scaremonger have, unsurprisingly, proven unable to deal with real threats. These include the steady decline in the ability to generate meaningful employment for gainful return, apathy and indifference towards the emerging devastation of the climate crisis and, of course, more dramatically, failures to control the spread and potency of the pandemic that has decimated societies. Those divisive formulas that won power, ostensibly in the name of the majorities, failed to evoke a response that could safeguard life, generate standards of living, or come to terms with the problematic histories that led to the call for #BlackLivesMatter.
The result is a loss of authority and respect for governance, tokenistic actions regarding the climate crisis, and eye-watering death tolls as individuals without the requisite governance experience find themselves out of their depth, but are not endowed with the spirit or courage to resign in realization of their own limitations. Rather they have decided to ‘fight back’: stirring more hate, deflecting blame while continuing to drive humanity towards disaster by inaction and ineptitude, ensuring only that they squeeze out profit for their wealthy friends with insatiable appetites.
This caricature of some democracies stands in sharp contrast to others. Covid-19 has served as a testing ground for the democratic health of many countries, particularly their ability to prioritize the safety and well-being of all their citizens regardless of religion, language or ethnicity. Societies that invested in generating and reconstructing an inclusive national fabric have facilitated the development of the collective talent present in the entirety of its society. These states, led by individuals (often women), listened to the unfolding crises carefully and hastened to ensure the pandemic would not spread. They did not worry about identities and entitlements, nor seek to construct bluffs or displays of bravado, resorting instead to long hours of meticulous planning to ensure that the entirety of their populations would come through the crisis. They realized the virus would not discriminate and put in place measures to ensure safety and security especially for the vulnerable, conscious that leaving the virus festering among subaltern communities would be not only morally dubious, it would effectively prolong the economic crisis that will inevitably follow to hinder compete eradication.
In many ways, the pandemic has brought to light many long-standing issues such as exclusion, inequality and invisibility that were already recognized in the Sustainable Development Goals (SDGs), with their emphasis on ‘leaving no one behind’. These are the key challenges for minority and indigenous rights in the next few decades, even once the devastation of the current pandemic has passed. While Covid-19 may become the defining crisis of the early twenty-first century, it looms against the larger, more entrenched environmental crisis: this, like the virus, is already impacting disproportionately on minorities and indigenous peoples.
The SDGs call for urgent action at scale in addressing planetary issues such as climate change through reducing consumption and reversing damage, while seeking solutions to benefit life in its entirety on the planet, including the seas; they focus on ensuring that people-oriented benefits – the end of poverty, equitable access to health, education and sustained work – accrue to all, with none left behind; and they outline a range of processes, including the active reduction of inequality, the elimination of gender disparity, and the entrenching of global solidarity and institutions to harness cooperation in achieving this vision.
The message for us at MRG is clear: we need to work actively in cooperation with others to out-think and out-manoeuvre the bullies that lurk ready to seize opportunities to enrich themselves, while actively designing solutions and systems that invest in the people that can replace them. One option saves lives here and now. The other is focused on winning the future in such a manner as to make the angry men irrelevant. Most crucially, this has to be done by educating majorities, schooling them in the ways of empathy – the same foundational value that led the smartest and hardiest to reach out beyond their worlds to others. This time we do not need saviours at high table, just the collective power and determination of the many, to imagine and implement solutions for a world where differentiated human identities are a source of celebration, not a red line between existence and annihilation.
Top photo: An elderly Nyangatom man in Omo valley, Ethiopia / Alamy
-
By Shaun Johnson
A book on my shelf that I especially treasure is titled David Astor and the Observer (David Astor was Editor of the Observer from 1948 to 1975). In it, the biographer Richard Cockett gives a fine account of the sweeping and significant life that was that of David Astor.
But the reason for my treasuring the 1991 edition above all is to do with the subject rather than the authorship. For David, in his elegantly evolved but characteristically somewhat diffident hand, had inscribed it thus at the time:
To Shaun
With thanks for getting me interested in politics again.
Yours, David
It is no secret among us legions of admirers and beneficiaries that David did, indeed, in later life get disillusioned and feel hopeless about what he often described to me as humans’ limitless ability to deceive themselves about their own actions in the services of right and wrong.
But how was it that I had the inestimable privilege of helping to get the great man reinvolved after a period of downcast withdrawal? In the mid-1980s he took me in to his home in Cavendish Avenue, St John’s Wood, after my time at Oxford ended and I contemplated the frightening prospect of going home to the fists and flames of my beloved, benighted South Africa. My country was then experiencing States of Emergency in what were (though we of course could not know it) the dying days of apartheid. He became fascinated once again by South Africa, with which he had been significantly engaged but had never visited.
David’s great friend Anthony Sampson, who had in fact introduced us, published a Festschrift in which this account was given:
In October 1986 David and Bridget spent a month in South Africa – his first visit to the country in which he and the Observer had been so long and intimately involved. They criss-crossed the country seeing famous anti-apartheid leaders on a State of Emergency tour planned and guided by Shaun Johnson, a young academic, writer and activist whom David had taken under his wing when he was studying in England on a Rhodes Scholarship, and who now worked on the Weekly Mail.
It was on this trip that I learnt of David’s seminal support for Minority Rights Group (MRG). I took him and Bridget to Durban to see his old friend and protégé Laurence Gandar, who had edited the now-defunct liberal Rand Daily Mail from 1957 to 1969 and who, after being sacked for alienating many of his white readers, moved to London (with David’s assistance) and became the first director of MRG. It was fascinating, all these years later, to listen to them reminisce about the early days of MRG.
David collected seemingly random causes, but in their globally far-flung range, you could always divine his logic when you worked out that in there someone, somewhere, somehow, was being done down unfairly. And when David Astor became convinced that someone somewhere was being done down, it was his unstoppable instinct to Somehow Do Something About It. MRG could not have dreamt up a more perfect champion and midwife if it tried.
Richard Cockett situates MRG in David’s body of works thus:
A practical illustration of David’s impartiality was the formation of the Minority Rights Group in 1961, an organization formed largely by him and Michael Scott to publicize the cause of oppressed minorities in the post-colonial world. The first director was Laurence Gandar. Others involved were Ronald Oliver, the Africa expert, and David Kessler, editor of the Jewish Chronicle. The Minority Rights Group produced studies of the plight of ethnic or national minority communities, whether they be Kurds, Palestinians or Eritreans…. The fight for the classic liberal causes of political rights and freedom thus extended from white colonial to post-colonial African or Asian rule.
Jeremy Lewis recorded the catalytic factors behind the establishment of MRG:
The Minority Rights Group stemmed from David’s and Michael Scott’s support for the Nagas, and reflected, in part, their belief that – in David’s words – ‘the United Nations, being an organization of governments, is a particularly inhospitable forum for the rights of minorities.’ Once again, it began life with a lunch…, attended by David, Michael Scott, Guy Wint and Conor Cruise O’Brien in 1962; David told Keith Kyle that it was set up ‘to act as a friend, adviser and introducer of minorities, without becoming their propagandist’.
David’s involvement in MRG lessened over time but in all the years I spent with or near him, he made it clear that it was one among his many initiatives of which he felt most proud. It is an honour for me to add these small recollections to this valuable volume, which David would have much enjoyed while habitually pooh-poohing his own contribution. That was David.
—
Shaun Johnson was Founding Executive Director of The Mandela Rhodes Foundation from 2003 to 2019. Besides being a renowned anti-apartheid journalist, he was also an internationally awarded author: his works include: Strange Days Indeed, the bestselling book on South Africa’s transition introduced by Nelson Mandela, and the novel The Native Commissioner, winner of numerous accolades including the Commonwealth Writers’ Prize for Best Book in Africa. The Leverhulme Mandela Rhodes Doctoral Scholarship has been renamed the Shaun Johnson Memorial Scholarship in honour of his legacy.
Johnson passed away in February 2020. He wrote this personal recollection of his friend David Astor, MRG’s founder, just months before he died.
Photo: David Astor
-
By Nicole Girard
The mandate of MRG has changed and evolved over the past couple of decades as the organization has redefined its approach to minority rights. Consistent throughout these changes, however, is the effort to realize the rights of the world’s most vulnerable. Yet our thinking on which groups constitute the most marginalized and how we reach them has come a long way since our inception.
The concept of ‘intersectional discrimination’ is now key to our work. In order to reach the most excluded groups, we have to understand how discrimination intersects on different axes of identity – for example, gender, sexuality, age, race, religion and disability. These are not experienced independently of one another, but together compound the experience of discrimination in the lived reality of a particular individual.
This understanding of discrimination, however, was not widely prevalent in the international human rights community until perhaps the early 2000s, and is still overlooked today. The Convention on the Elimination of Discrimination Against Women (CEDAW) does not include specific mention of how women’s experience of discrimination may be compounded on the basis of race or religion, for example. CEDAW, though ground-breaking, prioritized a ‘shared experience’ of gender-based discrimination that relegated consideration of race and other forms of intersectional discrimination to its margins.

A Tamil woman in Sri Lanka. MRG also struggled with incorporating intersectional thinking into our work. Some of our reports from the 1970s focused on women in specific regions of the world, such as Women in Sub-Saharan Africa, but did not in fact address minority women in particular, yet the reports were revolutionary in even considering the distinct experience of women from what was then commonly described as the ‘Third World’. So too our 1980 report on female genital mutilation (FGM) was published only one year after CEDAW came into force, at a time when the practice was largely unknown to an international audience and the dialogue surrounding the practice was frequently sensationalist and sometimes racist too. Yet the report did not analyse any specific factors of intersectional dimensions that might be at play.
‘Essentially, our predecessors were feeling that what they were doing was shining a spotlight on marginalized groups more generally,’ explains Carl Söderbergh, MRG’s Director of Policy and Communications. ‘This would mean, in terms of MRG’s original thinking, that it would be working with groups, whereas most other human rights NGOs were working on the rights of individuals.’
Considerations of multiple discrimination began to influence our work in the 1990s, when gender issues were considered in all new reports, while the release of a report on Muslim women in India in 1999,was the first of our publications to deal exclusively with the rights of women from one minority group. Nevertheless, the report was not framed using an intersectional discrimination lens. Our change in approach was marked by the release of the report Twa Women, Twa Rights in the Great Lakes Region of Africa in 2003. As the second sentence of the preface states: ‘Twa women suffer from double discrimination, because of their ethnicity and their gender. These forms of discrimination can intersect to devastating effect, as in the sexual violence experienced by Twa women in the context of armed conflicts in the region.’
Since then, intersectionality has been a cornerstone of our work, informing all of our programmes and publications. Our online multimedia resource on multiple discrimination, Life at the Margins, marks our fullest exploration so far of these issues and many of its manifestations throughout the world. Furthermore, we are currently running a project on the rights of people with disabilities belonging to minority and indigenous communities, gathering data and building coalitions to work on this overlooked and often ostracized segment of the population, and have recently initiated an indigenous women’s maternal health project in Africa and Asia, with plans to address a significant lack of data in this area. As we continue to refine our approach to reaching the most vulnerable, the sentiment expressed in 1984 by our then Chair of our International Council, Professor Roland Oliver, remains true: ‘The Minority Rights Group is not there to reform the world, but to enable the muffled voice to be heard.’
Top photo: Indigenous women stand outside next to a wall in Chimborazo, Ecuador / Stephen Reich
-
By Nicole Girard
MRG became involved with Tamils in Sri Lanka with our first report in the 1970s, with regular updates thereafter. By the time Neelan Tiruchelvam joined MRG’s International Council in 1994, MRG was establishing a South Asia regional programme involving him and Radhika Coomeraswami, who were joint Directors of the International Centre for Ethnic Studies in Colombo. Both were distinguished lawyers, with Neelan Tiruchelvam being a Tamil parliamentarian. In Nepal, March 1999, he was elected Chair of MRG’s Council but was assassinated just three months later because of his strong stand for minority rights and for proposing a peaceful resolution of the Sri Lankan conflict. His life and work for peace was celebrated in a statement by the UN Secretary General. He was succeeded on the Council by Radhika Coomeraswami, who was a strong advocate of women’s rights and children’s rights; she later served as the Under-Secretary-General of the United Nations, Special Representative for Children and Armed Conflict, drawing on her personal experience of conflict and wars.
In Sri Lanka as elsewhere, women’s experience of war is different from that of men: their gendered roles and responsibilities affect the way they endure and recover from conflict. For Tamil women, the conflict and its aftermath posed specific threats of economic insecurity and sexual violence, many suffering the impact of losing male family members to unsolved disappearances. Understanding this gendered impact of war was key to MRG’s arts intervention with Tamil women in Sri Lanka, exploring concepts of hope and reconciliation, to lay the groundwork for future justice and redress.
Although the protracted conflict between the Sri Lankan military and the LTTE (Liberation Tigers of Tamil Eelam) officially ended in 2009, 20,000 persons are still considered missing. Women have been at the forefront in demanding answers regarding the whereabouts of their loved ones, endlessly putting pressure on authorities and the various commissions that have been established to address these and other post-conflict justice and reconciliation issues. And yet, women’s experience of war and the plight of their loved ones have been side-lined throughout. While hundreds of Tamil women had testified at the government-mandated Lessons Learned and Reconciliation Commission between 2010 and 2011, women’s stories were consistently interrupted and brushed over by commissioners.
In 2013 MRG, in partnership with the local Women’s Action Network (WAN), decided to take an alternative approach – using arts and poetry to give women a space to explore their experiences of war and loss. This was something that, until then, they had been unable to access, either through formal justice mechanisms or other healing initiatives. ‘I have participated in several workshops and programmes regarding peace-building and livelihood improvement,’ one programme participant recalled:
They all called and forced [us] sometime to forget the past and walk ahead. It [the MRG project] is the only programme [that] called us to memorize and to accept the past. We had the chance to share the real pain and get free a bit.
The format of the programme involved four hours allocated to art and another three for poetry exercises. Despite having little experience with either art or poetry, the women were guided first through group-oriented exercises and then moved on to individual expression. Participants were asked to draw what reconciliation means to them and then were given the chance to explain their drawings and how they felt during the process. ‘I did not use my favourite colour green in this picture,’ a 24-year-old Christian Tamil woman explained, ‘because our situation is not green now. It is so very challenging. In 2008, my brother was kidnapped by some unknown people who came in a white van. We still have hopes that my brother is alive.’
MRG’s Deputy Director Claire Thomas afterwards reflected that participants rarely had the chance to really engage in artistic expression, and its nurturance ‘had made for a more meaningful and personal exploration of reconciliation than would have been the case through a more traditional discussion format’. Thousands of Tamil women have a similar story and yet they are still not being heard by authorities. Despite this, some women at the workshop continued to have hope in the future and the potential that ‘reconciliation’ might bring. As captured in one woman’s poem:
Love is reconciliation
Relationship is reconciliation
Reconciliation is like a flower with fragrance
Pleading you, reconciliation, come to us
We have an eye on you…
We have dreams…
Don’t pass as a dream… come alive…
Reconciliation… -
By Claire Thomas
Although human rights in essence date back centuries, if not millennia, human rights as a movement really began to take off in the 1960s and 1970s. MRG’s birth was therefore at a moment when many like-minded groups were founded and momentum was building in a range of areas. However, while the majority of human rights organizations were focusing on civil and political rights issues such as torture, political prisoners and freedom of expression, from its infancy MRG focused on access to socio-economic rights – in particular, the right to an equal, quality, appropriate education for all.
Socio-economic rights were, some argue, a casualty of the Cold War, with the Western powers keen to focus on civil rights, where their track record was generally somewhat better, whereas the Eastern bloc stressed full employment and universal access to public services such as education. However, between 1971 and 1991, MRG published no less than 25 titles that called for attention to equal rights to education for minorities and indigenous peoples. These covered a very wide range of peoples and situations, from indigenous Australians, the Chinese in South East Asia, Asians in East Africa, Tamils in Sri Lanka, Tibetans, Puerto Ricans in the US, Inuit in Canada, Saami in Lapland, peoples of Zimbabwe, and Armenians, Kurds and Palestinians, as well as Bedouins of the Negev in Israel and the Occupied Territories. In addition, by 1991, MRG had published two in-depth studies on educational themes: Teaching about Prejudice and Language, Literacy and Minorities. In the 1980s MRG initiated a London’s schools education project producing a range of educational materials for the classroom which led on to the highly successful Voices project in the 1990s.
This research led, in due course, to extensive programmes on the ground that aimed to address the deep-seated inequalities faced by minority and indigenous communities in educational access. MRG specifically sought out opportunities to intervene in countries where discrimination was occurring to challenge bias and inequality in educational provision, ensuring that barriers that kept minority, indigenous and migrant children from attending or completing education were reduced or removed. This was borne out in part by the many testimonies from members of minority, indigenous and migrant communities to MRG that education represented the best opportunity for themselves and their children to escape the cycle of poverty and persecution.
Since the early 1990s, our research, campaigns and interventions have tackled everything from pointing out severe underfunding in nursery school provision in Turkana in Kenya, to documenting and addressing Batwa children’s regular experience of racist bullying and abuse from both fellow pupils and at times, teachers in the Democratic Republic of Congo (DRC). We worked with partners in Pakistan and Indonesia, as part of community/expert-led steering groups to develop and lobby for the adoption of curricula that treated all religious groups in those countries with respect. We worked hard to develop new materials that did not include religiously discriminatory content, but also educational resources in which all communities were represented and valued. We documented and lobbied when the closure of minority-language university provision in Macedonia contributed to an outbreak of violent conflict. And we have consistently supported the efforts of Roma to access quality education across Europe, including submitting evidence and arguments in precedent-setting cases on the issue of segregated schools.
One would think that the right to education would be a relatively straightforward demand, both for communities and duty bearers. But while it is true that a campaign for equal education may be more likely to succeed than a quota of seats in parliament for a minority community, for example, the power imbalances and complex political trade-offs that impact on all states mean that achieving a fair allocation of educational budgets to minority provinces, or removing hateful content from national curricula, is much harder than it perhaps ought to be. Even on the community side, the situation is not straightforward, with some members resisting mainstream schooling as an implicit threat to their own culture and knowledge – a position that is understandable given the long history of assimilation or denigration many have experienced. MRG was involved in a UNESCO world conference on adult education in July 1997, where it facilitated the participation of minority and indigenous representatives. One indigenous activist from the Chepang community in Nepal discussed the work of their organization, Seacow, focusing on how it illustrated the need to recognize communities’ different learning systems. Essentially his argument can be summarized as: ‘Why should I send my child to your school to learn your knowledge – billions of people in the world can read and write. Our knowledge of the forest, its plants and animals, is unique and precious – if my children don’t learn it, it will be lost to humanity for ever.’ This kind of input has made MRG think very carefully about seeing education, particularly teaching in majority community knowledge and languages, as a panacea or a universal solution that we can adopt uncritically. This gives rise to a pause and acknowledgement (rarely voiced) that education can ‘do harm’ as well as good. What we need to do, then, is look not only at the extent to which marginalized communities can access public education but also the degree to which that education reflects and includes their own values, needs and aspirations.
Until today MRG has maintained its focus on education: current programmes include efforts to hold the devolved county governments in Kenya accountable for how they spend education budgets. In other countries, too, our work continues to enable minorities to access education fully and equally – most recently, with Roma mediators and local authorities in Ukraine. Where possible, we also seek to challenge boundaries and explore innovative methods to improve educational access, even in intractable and difficult contexts. One project in the troubled provincial capital of Quetta in Pakistan established ‘Bard of Peace’ clubs in schools, with the students taking up the role of ‘Bard’ and using poetry and art to generate critical thinking and reflection among pupils about religious diversity and respect for all. The students in the clubs went on to develop performances for other schools and community members on issues of social inclusion, respect for all religions and equality within Pakistan’s society.
Photo: Internally displaced children learning in Abkhazia, Georgia / Agnieszka Zielonka
-
By Rachel Warner
Voices was a series of dual-language booklets of autobiographical writing by young asylum seekers and refugees in London schools, published by MRG in the 1990s, to meet a growing need for materials that reflected the experience of young members of minority groups. The first three books, published in 1991, were by Eritrean, Somali and Kurdish school students, and the second set of four books, African Voices, published in 1995, were by students from Angola, Sudan, Uganda and Zaire (as was).
The books included drawings by the school students, photographs of their home country, maps, a fact box and a historical introduction for teachers. They were designed to be used mainly at Key Stages 3 and 4 of the National Curriculum, for English teachers encouraging autobiographical writing, for citizenship education, and as a resource for teachers of English as an Additional Language (EAL) looking for relevant materials to use with school students and adults learning English. They included detailed activity suggestions for teachers.
The books were very well received, as this review in WUS News (March 1992) shows:
The series comes at an appropriate time. It can help counter racist attacks in the tabloid press that have tried to present the majority of refugees applying for asylum as ‘bogus’. Voices shows the tragedy of disrupted lives, of suffering and of the loss of childhood. This is the truer picture – the one the press should be presenting, in which ordinary people are swept up by events over which they have no control.… This series gives refugees an opportunity to speak. It is especially poignant that it is through the voices of children that their case is made.
Tom Deveson, in the Times Educational Supplement (10 November 1995), commented: ‘This excellent series of books … should be in every school and required reading for Cabinet Ministers … and editors whose noise is in inverse ratio to their knowledge or human sympathy.’
As much as the usefulness and success of the finished books, the way of producing them was significant – involving young people and community groups at all stages of the process. Meetings were held with relevant refugee organizations at the start of the project – for example, with the Kurdish Cultural Centre, Somali Education Project and Uganda Community Association in Lambeth, as well as with the Refugee Council and Medical Foundation for the Care of Victims of Torture. It was important that the school students were asked to share their (often painful) experiences by someone they knew and trusted – usually an EAL teacher in their school. Most stories were written – either in English or the student’s first language – but some were oral accounts. All contributors checked their edited account before inclusion, and members of the community checked the books at all stages of production. All the stories were translated into the language chosen by the young contributor and presented in dual-language format. This gave the minority language(s) status in the books, and meant, for example, that Voices from Uganda included six languages in addition to English. In total, 16 different minority languages were included in the books, ranging from Tigrinya to Dinka, Acholi to Lingala, Kurdish to Arabic.
The process of producing the books was shared with many teachers – mostly in London – who attended workshops about the books and were encouraged to get their own refugee pupils to write about their experiences and produce ‘in-school’ collections of writing. It was also the inspiration for an innovative project in 2006 in Tower Hamlets, where young Somalis interviewed their own parents, leading to a publication ‘When You Lived in Somalia …’
As well as detailing some of the traumas that the young people had experienced, leading them to become asylum seekers in the first place, all the Voices books contained positive memories of the countries the young people had left. For example, a 15-year-old girl from Zaire wrote, ‘I remember us picking mangoes when the season came for the fruits to be ready. We ate most of them, but not all. There were too many.’ A 16-year-old boy from Eritrea wrote, ‘Usually I went to the cinema [in Asmara] with six or seven of my friends. We sat upstairs and made lots of noise. We were imitating the actions we saw on the film, and shouting and clapping.’
The horrors were not far away, however. A 9-year-old Somali girl in an oral account said, ‘I remember that soldiers opened fire on the kids and other people. There was a lot of screaming and crying. Pupils were falling down all around me. It was like being in a nightmare.’ A 9-year-old Angolan boy said, ‘The soldiers killed my friend Mikali. They put her by the wall and shot her. She was my friend.’
All of the books end with accounts of the difficult journeys undertaken by the young people and their families to get from their home country to Britain, and comments on settling in Britain and their new life in the country. These accounts show such resilience – for example, a 15-year-old Ugandan girl wrote, ‘I feel very happy because I was rescued from death. I could have been killed. I don’t feel like going back to my country because I am still afraid. But I would like to help in some way.’ Another (14-year-old) Ugandan girl wrote, ‘I’ve learnt to read, write and speak English better. I’ve made friends.’ And a 12-year-old Kurdish boy wrote, `I stopped crying all the time and I had a feeling things were going to work out.’
Photo: Batwa women in Uganda / MRG/Emma Eastwood
-
From the beginning, MRG has systematically focused on health services and the barriers that minorities and indigenous peoples face in accessing them. The disparities, while often overlooked, are striking: where statistics are available, health outcomes consistently show that members of marginalized communities are less healthy, die earlier and use health services less frequently than other groups. This is the case not only in contexts where services are limited and resources scarce, but also in affluent countries with well-funded health systems. In the UK, for instance, research suggests that black males have a life expectancy four years lower than their white peers.
As with education, health services are often difficult for minority and indigenous communities to access, with many barriers to equitable access in place. These include geography, with many communities situated in remote locations, far from capital cities and with little or no infrastructure in place. Language diversity and the frequent lack of comprehensible information also contribute to health inequalities. An added challenge is the widespread absence of disaggregated data on the specific situation of minority and indigenous communities – as a result, critical shortages of even basic health care can end up being concealed in national averages or overlooked altogether from official surveys.
But these challenges, which also reflect wider issues of discrimination and exclusion, can all be solved given political will. Sadly, minorities and indigenous people often have very little – if any – voice in political decision-making, including health budget allocations and priorities. At a local level, minority and indigenous communities often have no say in the design of services, which as a result can be established using a ‘one size fits all’ approach that may be culturally unacceptable: in Ethiopia, for example, painting clinics white (a colour associated with death among some communities) is one example of culturally insensitive design that was shown to have impacted on women’s willingness to access maternal health services.
Sadly, discrimination in health services can be even more direct. Minority and indigenous men and women still report first-hand experiences of explicit racism from clinic staff: from Batwa in the Great Lakes region to minority clan members in Somali IDP (internally displaced person) camps, MRG has documented numerous examples of members of marginalized communities being denied access by the very people who should be helping them. The treatment of Roma across Europe is especially disturbing. One area MRG has lobbied on was the practice of forced sterilization of Roma women in some Eastern European countries, after reports emerged on this shocking issue – a legacy of the Communist era that, while officially prohibited in the early 1990s, continued to occur more than a decade later.
Still, we have found that if we support and train activists to make advocacy claims in compelling ways, results can be achieved, against the odds. For instance, MRG was one of the first organizations to do extensive work on the practice of female genital mutilation (FGM). At the time, much of the limited coverage of this issue was coloured by stigma and misconceptions that did little to engage with the challenge of ending its devastating impacts on girls. FGM is not a minority and indigenous issue per se, as many majority community women have also been affected in different contexts. However, for communities whose culture and way of life more generally had long been dismissed or denigrated, anti-FGM campaigning could be seen as just another example of hostility towards them – even when the need in this case for urgent change was overwhelming.
Of course, we all know (now) that work to tackle FGM and similar practices needs to begin and be led by minority and indigenous women themselves, whose efforts are not dismissed as ‘yet another attack’ by outsiders. MRG’s policy of focusing on activists working directly with communities helped to achieve real impact here. This is illustrated by the legacy of Efua Dorkenoo, a highly respected British-Ghanaian campaigner who wrote one of the first reports on FGM, MRG’s Female Circumcision, Excision, and Infibulation (1980), and would later follow this with a full-length book with MRG in 1994, Cutting the Rose, when she was an MRG Council member. This book was selected by an international jury in 2002 as one of ‘Africa’s 100 best books of the 20th century’. While working with MRG, she coordinated the UK-based Women’s Action Group for Female Excision and Infibulation (WAGFEI) and travelled to a number of FGM-affected countries in Africa. Her example demonstrates how much more can be achieved in transforming health by engaging effectively, as Efua did, with those most affected.
MRG’s work on health builds on the ground-breaking research that we have undertaken over the years on behalf of communities, ranging from Palestinians in the Occupied Territories to asylum seekers in the UK. Unusually, from early on MRG also focused on mental health with reports like The Rights of Mentally Ill People (1987). This reflected our recognition that the experience of stigmatization and invisibility that many communities faced on a daily basis frequently exacted a heavy psychological toll. In more recent years, MRG has continued to develop research on health. In 2013, for instance, our flagship publication at the time, State of the World’s Minorities and Indigenous Peoples, was themed around health.
One issue that MRG has consistently championed is the need for inclusive, disaggregated data for minorities, indigenous peoples and other excluded groups. Developing clear evidence to show the reality of health inequalities on the ground is often the first step to achieving change. In 2017, we co-researched an analysis of indigenous women’s and girls’ access to maternal and sexual health services, commissioned and published by UN Women, UNICEF and UNFPA. This showed that even in the era of the SDGs and their call to ‘leave no one behind’, the limited statistics available showed that indigenous women were significantly less likely to access health services. For some communities the figures were particularly stark, with indigenous women more than three times more likely than other women to have received no ante-natal check-ups. What made this situation even more worrying was the fact that out of 90 major health surveys, only 16 had collected data on indigenous women – meaning that in many, many other states no information on this was available at all.
MRG’s latest work on health has focused on training minority and indigenous community activists to understand and challenge the health budgets that are decided upon for their communities. We believe this will allow them to demand services that work for them and budget allocations that are fair, allowing health services to reach those who need them.
Photo: Somali women walking in Mandera market on the Kenyan side of the Kenyan Somali border / Kim Haughton/Alamy
-
By Claire Thomas
A recent and ongoing example of MRG’s work on health focuses on minority and indigenous women in Cambodia, Ethiopia, Kenya and Myanmar and their right to equally access sexual and reproductive health services such as contraception, pre-natal care and skilled attendance during birth. This project (funded by the UK government and run in partnership with Health Poverty Action) has three phases: first, to understand the extent to which women in minority and indigenous communities access these health services less than women nationally and why; second, to run pilot projects to tackle the barriers that are preventing women from accessing services; and, finally, to lobby for wider adoption of the successful pilot project methods so that more women benefit from these innovations. At the time of writing we are in the first phase of this project.
Some initial research focused on Mandera County in north-eastern Kenya, populated almost entirely by members of the Somali minority, has highlighted striking disparities in terms of access to essential care. Our surveys found that Somali women there were much less likely to access contraception (a shocking 1.9 per cent compared to the national rate of 58 per cent), significantly less likely to attend four ante-natal care appointments (37 per cent compared to 58 per cent nationally) and less likely to access skilled attendance at birth (39 per cent compared to 62 per cent nationally). Is it any wonder that the maternal mortality ratio in Mandera County in 2014 was 3,795 for every 100,000 live births – more than 10 times higher than the national average (362 for every 100,000 live births)?
MRG’s project has trained Somali women in Mandera to interview women within the community about why they do not or cannot access services. We believe that when Somali women themselves ask the questions, the women are more honest than they would be with an external researcher about the factors that prevent them from accessing services. Some reasons are to do with lack of provision or staffing in clinics, but some are to do with religious and cultural beliefs which women may be reluctant to discuss frankly with people from outside the community. Interviews have been carried out with 160 women and the results are being compiled. We will use this new understanding about the real barriers to accessing services, developed from within the community, to design pilot projects aiming to transform the situation.
In a linked piece of work, MRG carried out research for UNFPA on the same topic. This research analysed the data that was available globally on whether and why indigenous women access sexual and reproductive health service less than other women. We analysed 90 global surveys run by either USAID or UNICEF, which led on global health data collection. Of 90 surveys, only 8 had published data that showed whether indigenous women were able to access health services equitably. A further set of surveys had gathered that data but not published it, which we then analysed. In the end we were able to show that in the 16 cases where data existed, indigenous women were always less likely to be accessing services than the national average. This did not surprise us, but what did surprise us was the ongoing resistance to including questions about ethnicity in such surveys and publishing the findings.
MRG believes that to address a problem, you need to first collect the data and to do that you need to know which communities are benefitting from interventions or are being excluded. If you do not gather that data, or ask those questions, then you will never understand why disadvantage and discrimination are happening. And until you understand it, efforts to address it are like stabs in the dark. It is clear that, despite the fact that five years have passed since the international community committed through the 2030 Sustainable Development Agenda to ensure that ‘no one is left behind’, we all have some way to go before we can claim to have delivered on that promise.
Photo: Minority woman in Somalia / Susan Shulman
-
By Neil Clarke
MRG’s work with the UN has been one of the cornerstones of its work and identity over the last 50 years. The organization’s profile as the leading international non-governmental organization (NGO) in the field of minority rights has meant that MRG has been the ‘go-to’ organization in the development of international minority rights standards and their implementation.
Pre-dating the UN, the League of Nations, founded in 1920, had the protection of minorities as a central aim of its mandate. However, following the Second World War and the founding of the UN with its key document, the UN Declaration on Human Rights, followed by a succession of other treaties, detailed reference to the rights of minorities was far more limited. This was the result of sensitivity regarding how the claims of ethnic and religious minorities might provide a casus belli for states to engage in further conflict. However, in time, it became increasingly clear that the existing norms were insufficient for the protection of minority rights and a long process began, though little progress was made on this initially with some states being adamantly opposed to recognizing the existence of minorities.
In 1989, a new order began to emerge with the new democracies in Eastern Europe, the collapse of the Soviet Union and the end of the Cold War. In the 1990s, MRG became heavily involved in the CSCE/OSCE processes, involving 51 states. It was a period of hope but old fears loomed not far away.
MRG, in partnership with the Helsinki Committees, organized major conferences in Copenhagen and Leningrad to promote a democratic and minority rights-based approach to these latent conflicts. Central to these two conferences was the engagement of civil society, including minority representatives, government officials and international scholars. The recommendations of the conferences and the mobilization of minorities directly influenced the OSCE minority rights regimes adopted in Copenhagen in June 1990 and provided a new momentum and agreed language for making progress on the text at the UN of the Declaration on the Rights of Persons Belonging to National or Ethnic, Religious and Linguistic Minorities.
MRG emerged as the key civil society counterpart to government representatives at the UN during the negotiation of the text, utilizing its own expertise, led by Patrick Thornberry (later to become Chair of MRG’s International Council from 1998 to 2002) and drawing heavily on its own close discussions with minorities. Subsequently, MRG provided a platform for minority activists from around the world to argue for the adoption of the UN Declaration and the establishment of a mechanism to promote its implementation.
Eventually, in 1996, a UN Working Group on Minorities was established where MRG organized the advocacy training and facilitated the participation of representatives of minority communities. Throughout the next two decades MRG continued to play a key role in shaping international minority rights norms, not only at the UN but also within European mechanisms, leading to the adoption of the Council of Europe (CoE)’s Framework Convention for the Protection of National Minorities and the founding of the OSCE’s Office of the High Commissioner on National Minorities.
Throughout the last 50 years, one of the crucial areas of engagement of MRG has been in promoting the implementation of minority rights. A Director and then a Council member were independent expert members of the UN Sub-Commission on the Prevention of Discrimination and Protection of Minorities. Another Director was the President of the CoE Advisory Committee on the Framework Convention for the Protection of National Minorities (FCNM); two of our Chairpersons have been members of the UN Committee on the Elimination of all forms of Racial Discrimination (CERD); and a member of MRG’s International Council has chaired the United Nations Expert Mechanism of the Rights of Indigenous Peoples (EMRIP),
A further highlight of MRG’s 50-year track record in international advocacy was its role in leading civil society lobbying for the creation in 2006 of the role of the UN Independent Expert on minority issues, subsequently renamed as the UN Special Rapporteur on minority issues, and then the establishment of the UN Forum on Minority Issues the following year, after a campaign led by MRG and the International Movement Against all Forms of Discrimination and Racism (IMADR). The success of the campaign for adoption was very much against the odds: indeed during the UN reform process that took place in the mid-2000s, it was feared that a space for minorities at the UN would be abolished altogether. The success of the campaign lay mainly in the coalition of 80 largely minority-led civil society organizations (CSOs) from around the world, which MRG and IMADR were able to convene, all of which engaged in lobbying and the drafting of recommendations.
However, it is not the architecture of the UN or the international normative system that is at the heart of MRG’s engagement – it is in ensuring that the presence and voices of minority activists and communities are seen and heard on the international stage and, most crucially, that these platforms can be used by activists to effect real change for their communities. Indeed, many of the CSOs which supported the campaign for the establishment of the Forum were graduates of MRG’s annual training program on UN advocacy, now running in Geneva for close to 25 years, often in cooperation with the OHCHR (Office of the UN High Commissioner for Human Rights) Minority Fellowship Programme. These days the training specifically precedes the Forum in November each year, allowing participants to attend the event and apply their skills through active participation. Sadly, the accessibility of the Forum to minority activists is still limited, due to the failure of the UN to provide adequate funding. So MRG’s support to activists, particularly those from the global south, has been critical in ensuring the genuine presence of minorities at the UN.
There are now several other international organizations engaging with minority rights at the UN, particularly within the normative framework and development of the Forum. However, our focus on practical advocacy and strategic use of UN mechanisms, in cooperation with partners, is still unique. Indeed, while there is genuine reason for scepticism as to whether UN mechanisms are able to influence change for minority communities, our partners find different and unique values in the process. Often their presence at a UN meeting can enable a minority activist to engage in direct dialogue with a government official or create media visibility for the issues they face – opportunities that may be unavailable to them at the national level. Besides finding crucial allies and partnerships through networking opportunities they would not normally have access to, participation at a UN event can also be greatly empowering in its own right for our partners, not to mention members of MRG’s own team.
Photo: MRG staff and partners at the UN Forum for Minority Issues in Geneva, Switzerland, in November 2019
-
By Evelin Verhás
By the early 2000s, the indigenous peoples’ rights movement had successfully achieved the creation of several UN mechanisms devoted to indigenous issues, including a Working Group, a Permanent Forum and a Special Rapporteur. In contrast, the Working Group on Minorities (WGM) was the only UN mechanism exclusively dealing with minority issues. The role of the WGM was crucial in providing a platform for minorities to have a voice within the UN system, take part in policy debates and engage in dialogue with states. However, its expert-dominated agenda and limited mandate created frustration among minority representatives as they increasingly felt that their specific concerns remained unaddressed.
In an attempt to address these shortcomings, following a series of consultations with its local partner organizations, MRG launched a campaign, with support from other international NGOs, to establish a new mandate: the Special Representative of the Secretary General on Minorities (SRSG). It was envisioned that the SRSG would complement the work of the WGM and have a mandate focused on conflict prevention. By sending communications to governments and conducting country visits, the SRSG would monitor specific situations and engage with governments in a constructive manner in order to resolve issues causing tension between them and minority communities.
After gaining the support of key stakeholders, including the government of Austria, the OHCHR Indigenous Peoples and Minorities Section, as well as the WGM, the campaign concentrated on targeting member states of the Commission on Human Rights (CHR) to ensure that the draft resolution calling for the creation of an SRSG put forward by Austria would pass. During the discussions at the CHR meeting, the focus on conflict prevention was deleted from the wording of resolution and it was agreed that the new mechanism would be called an Independent Expert on minority issues (IEMI).
In April 2005, the CHR resolution 2005/79 established a new special procedure, and Gay McDougall (who would go on to become Chair of MRG’s International Council from 2014 to 2020) was appointed IEMI by the High Commissioner for Human Rights in July 2005. As the first IEMI, she had the opportunity to play a crucial role in shaping the new mandate. She aimed, as she put it, ‘to give the mandate and the Declaration a global face and perspectives, and to give the issue of minority rights a twenty-first-century makeover’.
McDougall clarified the normative foundations of the mandate, articulated some definitional issues and outlined the scope of application of minority rights. She also identified thematic priorities for her work in response to the current situation of minorities. Recognizing the relationship between discrimination and poverty, she sought to increase the attention paid to minority communities in the context of poverty alleviation and development. She addressed extreme measures of exclusion, such as discriminatory denial or deprivation of citizenship, and emphasized the role of minority rights protection in preventing conflicts and promoting stability. She also worked towards mainstreaming minority issues at the UN and increasing cooperation with UN specialized agencies, treaty bodies and other human rights mechanisms.
In her six years, the IEMI sent numerous communications to governments regarding their failure to fulfil obligations to protect the rights of minorities. McDougall also carried out 12 official country visits, affording opportunities to strengthen the link between minorities and the UN. During each visit she met with minority organizations, communities and representatives, including minority women, listened to their concerns and then took these up the governments, incorporating them into her mission reports as appropriate.
In 2007, the Human Rights Council (HRC) adopted a resolution establishing the UN Forum on Minority Issues, replacing the WGM, to ‘provide a platform for promoting dialogue and cooperation on minority issues’ as well as ‘thematic contributions and expertise to the work’ of the IEMI. The IEMI was charged with guiding the work of the Forum and invited to incorporate the forum’s recommendations into her reports to the HRC.
The establishment of the Forum created the opportunity to present minority voices not only as victims describing violations but also as experts involved in formulating solutions. The IEMI also ensured that the Forum’s annual outcome documents reflected the views and recommendations of all Forum participants, including in particular those of minority communities, so the usual government-negotiated language focusing on minimum standards was avoided. Under McDougall’s guidance, the Forum became what it is today, namely an important platform for amplifying minority voices at the UN and strengthening the participation of minorities in assessing and developing international guidelines and policies aiming to improve their situation on the ground.
Photo: Ludovic Courtès, CC BY-SA 3.0, via Wikimedia Commons
-
By Peter Grant
In 1970, shortly after our foundation, MRG launched our first publication: Religious Minorities in the Soviet Union. This was followed shortly after by other reports, ranging from the situation of Aboriginal Australians and that of Ainu, Burakumin and Koreans in Japan, to Asian minorities in East and Central Africa and human rights in ‘Eritrea and Southern Sudan’ (long before either region achieved independence). This snapshot offers a small glimpse of the sheer breadth and diversity of the hundreds of reports, books and briefings that have come in their wake.
Research has always played a central role in MRG’s work. In many cases, these publications helped document the challenges facing communities whose predicaments might otherwise have gone unreported. From media engagement to public advocacy, they were instrumental in achieving some of the organization’s first successes and continue to shape its activities to this day. For academics, journalists, policy-makers and, most importantly, for the communities themselves, these resources have helped to highlight the discrimination, exclusion and stigma that still define the lives of so many groups worldwide.
From the beginning, the impact of MRG’s publications was considerable. Its second ever report, The Two Irelands: The Double Minority (1971), was praised on publication for its balanced assessment of a situation too often presented in highly partisan terms. Described by Chatham House as ‘the best pages on Ireland’s contemporary political problems that have found their way into contemporary literature’, the report was credited with having an enduring impact and was still shaping discussions surrounding the Good Friday Agreement more than 25 years later. In 1997, MRG launched the book Scorpions in the Bottle: Conflicting Cultures in Northern Ireland, by John Darby (the founding Professor at the UNU International Conflict Research Institute (INCORE) in Belfast) at its international conference in London. This was accompanied by speeches from the Irish ambassador and a spokesperson of the British government’s Northern Ireland Office, both of whom commended MRG’s publications and referred to the inter-governmental discussions that were then underway.
MRG was also one of the first organizations to produce an accessible account of the Armenian genocide for an international readership. The report, The Armenians, was first published in 1976 and updated on a number of occasions over the following decade. This work was awarded the United Nations Association Media Peace Prize in 1982 for shining a light on this ‘hidden holocaust’ and the legacy of discrimination that Armenians were still experiencing in Turkey. Many of MRG’s other reports were also similarly ground-breaking in documenting the situations of communities which, at the time, had often received little or no coverage even in their own countries.
Perhaps the central achievement of our reports over the years has been to challenge the invisibility and silence that generations of minorities and indigenous peoples across the world have endured. Unseen and unheard, governments, armies, landowners and corporations have been able to exploit them in part because in many cases the communities have not even officially been recognised. When MRG published No Longer Invisible: Afro-Latin Americans Today in 1995, for instance, Afro-descendant populations in many parts of Latin America were still not included in national censuses. Increasingly, now, these communities are being acknowledged, and self-identification is growing after decades of assimilation. More recently, our 2015 online multimedia resource, Afro-Descendants: A Global Picture, drew attention to the presence of Afro-descendant communities in Asia, Europe and the Middle East, many of which are still struggling for recognition.
MRG has remained at the forefront of the discussions around minority and indigenous rights, with its World Directory of Minorities and Indigenous Peoples, first published in 1990 and then developed further in 1997 as a reference book and currently being updated in its online format, still regarded as the most authoritative resource in this area. MRG has also produced regular annual reports that have covered some of the most urgent concerns of the time, with recent volumes exploring urbanization, migration and climate change. These publications have both reflected and anticipated the changing human rights environment for minority and indigenous communities. As these challenges have evolved, so too has MRG’s approach to its research, with communities playing an increasingly central role as partners, rapporteurs and authors in describing their situations and articulating their own needs to national governments and the international community.
While looking through the back catalogue of MRG’s reports can provide many examples of hard-fought progress, it is also a salutary reminder that the struggle for justice and equality is rarely over. From Roma in Europe to Haitians in the United States, many of the groups we were working with decades ago are still experiencing the same problems today – or have new challenges that make their situation even more precarious. But it is also true that, without MRG’s reporting, the challenges facing many of these communities would not even be under discussion, and that is what will continue to drive our research in the decades to come – the need to ensure these communities are seen and heard.
Photo: Collage of report covers produced by Minority Rights Group in the 1970s-1980s
-
By Alan Phillips
The year 1989 was a watershed for minority rights in Europe. The tearing down of the Berlin Wall in Germany symbolized the rejection of the Communist system by the people of Central and Eastern Europe. Although MRG was a very small organization then, it responded speedily and effectively, drawing on its expertise, reputation and strong links with minority communities. On the one hand, there was an extraordinary atmosphere of change sweeping through Europe but also fear, particularly among western governments, that there was a strong possibility of violent inter-ethnic and inter-state conflicts mobilized by nationalist politicians.
MRG realized that it was time for a radical change in its approach. Over the previous two decades it had published a substantial series of printed reports, most of them around 20,000 words – short enough to be read in an evening. These were written by respected journalists and academics, and achieved an excellent reputation for their accuracy and analysis that attracted a wide readership. By 1989 there were already 80 titles with 440,000 copies sold over the previous 20 years. MRG adopted a radical new strategy of advocating minority rights in international forums, by promoting new international standards on minority rights and by targeting its publications to support this advocacy.
Crucially, it decided to publish a comprehensive new volume, The World Directory of Minorities: drawing on its rich library of reports and with the support of its network of authoritative experts, it synthesized its existing research, supplemented it with many new contributions and documented key minority rights standards. The concept was developed with the major publisher Longman to maximize its global outreach. MRG had already published three little known, short paperbacks, the first in 1977, with descriptions on ‘World Minorities’ that, while dated, provided a useful blueprint.
The World Directory of Minorities was published in 1990 with 160 major entries covering hundreds of named minorities. It also included major national and international standards on minority rights. It was a ground-breaking reference book designed to reach out well beyond academics, students and the UK press to an international audience of decision-makers in governments and intergovernmental agencies, including the UN Commission on Human Rights.
The directory never claimed to be comprehensive, nor was it suggested that it could be totally objective. Although it was a substantial hardback book of over 450 pages, it was based on entries that had been well researched and peer reviewed to ensure that it provided valuable, reliable information and promoted a greater understanding of the circumstances of minorities. The intention was to produce a living directory and, in the first editions, MRG strongly encouraged researchers to make contact if they could introduce us to a body of research that would ensure a more comprehensive coverage in future. It was seen as work in progress.
The first edition was widely acclaimed and was reprinted in 1991. It was costly to publish in a book form, but a new edition extending to over 800 pages was published in 1997. By then, the directory had played a significant role, not only in documenting the situation of minorities, but also in enhancing the reputation of MRG and adding to its authority. MRG used this in promoting the CSCE/OSCE standards on minorities (1990) and also in promoting the UN Declaration on the Rights of Minorities (1992), which subsequently inspired the Council of Europe’s (CoE’s) Framework Convention for the Protection of National Minorities (1995), and the crucial UN and CoE monitoring mechanisms.
The directory, now known as the World Directory on Minorities and Indigenous Peoples, has for the last decade been an online reference and was recently updated again with new entries. It will now be regularly refreshed to include recent developments and remain relevant for the policy-makers, academics, journalists, activists and others who rely on it for information. With thousands of unique users each year, it is one of MRG’s most widely used publications today – a testament to the lasting value of this resource three decades on.
-
By Hamimu Masudi
The dubious origins of statehood in Africa have been clear to anyone interested in understanding and explaining contemporary development challenges on the continent. By the stroke of a pen at a Berlin conference in 1884, the entire continent was fragmented into 53 multiethnic states, subsequently governed under imperial rule for over 60 years. Even though it was evident that the millions of Africans across the continent were extraordinarily varied in their cultures and ways of life, different population groups – often with a history of intercommunal conflict – were forced to live together under administrative systems that favored certain lifestyles and discriminated against others.
Due to their distinct cultures, ethnic minorities and indigenous peoples including nomadic pastoralists, hunters and gatherers were particularly sidelined throughout the colonial period, in the process losing their lands, livelihoods and dignity. Sadly, the end of colonialism did not restore order and liberty for all. Instead, it ushered in a crop of authoritarian African strongmen who were happy to perpetuate the exploitative policies and institutions of colonialism for their own ends.
This is illustrated by the continued plight of forest peoples in many countries who, without any sort of compensation, have seen their forests and grazing areas taken from them and gazetted as public land – often on the dubious basis that they normally do not own permanent physical structures nor tend to any crops on the lands. The same arguments were made in order to explain the displacement of pastoralist communities. Consequently, entire populations have been evicted from their territories, leaving them to eke out a marginal existence on the periphery of the lands they once called home.
It is against this background and the desire to address persisting inequalities that MRG has conceptualized and implemented its work in Africa over the years. From programmes responding directly to the urgent health and educational needs of communities, to defending collective land rights and advocating for legal recognition, MRG has over time influenced the understanding and perception of minorities and indigenous peoples on the continent.
For instance, in view of the widespread belief that all inhabitants are indigenous to Africa, most governments have neglected to identify or recognise indigenous peoples in their territories – a situation that has held back the legal recognition of their rights. In response, since the launch of the Africa office in Kampala, Uganda in 2001, MRG has successfully challenged these narratives, arguing instead that the situation of minorities and indigenous peoples is distinct, and that the discrimination they face threatens their particular cultures and reinforces their subordinate position within social and state structures.
This subordinate position has an even more severe impact on vulnerable groups within minority and indigenous communities. Since its very earliest days, MRG’s Africa office has applied an intersectional lens to its work, for instance by providing support to Batwa activists across the Great Lakes region who are combatting violence against women and gender-based discrimination. Currently, MRG is building on and expanding this work by supporting Batwa who are seeking recognition for the rights of persons with disabilities belonging to their communities.
The rights of Africa’s minorities and indigenous peoples should be protected and promoted alongside other national priorities, such as environmental management and nation-building. Fortunately, there is now increasing acceptance that indigenous peoples, including pastoralist communities, value their natural surroundings more than anyone, given their close and centurieslong interdependence with their lands, and that indigenous knowledge is central to any successful conservation strategies in Africa. These arguments have at least led to some initial recognition of minority and indigenous rights – an important milestone, given that community evictions are still justified by many governments in the name of environmental protection.
In particular, it is through the judiciary that the struggle for recognition and respect for indigenous peoples’ rights is being waged in Africa. From Kenya and Uganda to Burundi and the Democratic Republic of Congo (DRC), law courts as well regional bodies such as the African Commission on Human and Peoples’ Rights and the African Court on Human and Peoples’ Rights have delivered significant victories in the battle for indigenous rights. These include the Ogiek and the Endorois victories at the regional level against the Kenyan government, the Twa family land case win against powerful individuals in Burundi, the Benet of Mount Elgon petition for social protection in Uganda and the Mbute of DRC’s Ituri Forest’s legal challenge for protection.
Now, thanks to the advocacy efforts of MRG’s partners, Burundi’s constitution provides for special representation of Batwa people in the National Assembly and the Senate, while Kenya’s constitution (under the Bill of Rights) guarantees the protection of minorities and other marginalized groups, and its land law further provides for collective land rights. And for the first time in their respective histories, members of the Batwa communities of Burundi and Rwanda have been appointed as ministers to Cabinet-level positions in their respective countries.
Photo: Members of the Sengwer community protest their eviction from their ancestral lands in the Embobut Forest, by the Kenyan government / Katy Migiro/Reuters
-
By Chris Chapman
Providing support to minority and indigenous representatives has always been a central part of the MRG ethos. For many years the organization has been running training workshops for activists, first in Geneva and Strasbourg, and later in countries such as Iraq, Egypt, Kyrgyzstan, Cameroon and Costa Rica. This work continues to this day and is integral to MRG’s strategy of achieving lasting impact in the countries where it works.
The programmes in Geneva and Strasbourg focused on sharing information and know-how about the human rights conventions and declarations that states have signed up to, and how the institutions in those places (the UN and the Council of Europe respectively) can be used to put pressure on states to respect the commitments they have made. These workshops were typical of MRG’s capacity-building work for some years, and had an invaluable impact, but there was a growing realization that activists also needed skills in other areas – in particular, leadership, fundraising and campaigning. In 1998, MRG began pioneering a regional training programmes in Budapest for minority activists producing an advocacy training manual.
This reflects a process of what might be called the decentralization of human rights advocacy. Although international NGOs are now increasingly becoming truly global, with offices and staff in many countries around the world, human rights violators try to brush off their advocacy efforts, pointing to the origins of many of these organizations in the global north and dismissing them as neo-colonial meddlers. Meanwhile, grassroots activism is on the rise and is finding new ways to pressure governments. If there is any doubt about this, you need only look at the epidemic of national laws that aim to stifle locally based NGOs and cut off their sources of funding, from Hungary to Israel, from Russia to Ethiopia, from Ecuador to Cambodia – illustrating very clearly the challenge that a vibrant civil society poses to governments that violate human rights norms.
To reflect this trend, MRG is finding new ways to build capacity, including online training, a programme which now has upwards of 1,200 alumni. In Mauritania, innovative ways needed to be found to get around government foot-dragging on the elimination of slavery conditions endured by the Haratine minority. International condemnation had pushed the government to adopt anti-slavery laws, first declaring the practice abolished in 1981, and then criminalizing it in 2007. However, social attitudes around slavery remained entrenched, and the government was reluctant to put slave-owners in prison. Although tough sentences were passed, they were often overturned on appeal, with slave-owners fleeing to neighbouring countries. MRG worked with partners such as Anti-Slavery International and the Mauritanian organization SOS Esclaves on a programme to push for the criminalization law to be implemented. As well as lobbying the government both in-country and in international settings, such as the African Commission on Human and Peoples’ Rights in Gambia, the partners embarked on an ambitious programme of training, not just for NGOs like SOS Esclaves, but also for Haratine activists, magistrates who would be hearing slavery cases, lawyers and paralegals to support victims in courts, and journalists to help with changing social attitudes.
The programme had to adapt to the government’s evasion tactics. After magistrates had been trained on the anti-slavery law and the relevant international human rights obligations, they were moved to courts covering other issues. So the partners shifted their focus to lawyers, paralegals and activists, who were more likely to engage on the issue on a long-term basis. One of the notable outcomes of this programme was a ruling by the African Union’s child rights committee in 2018 in favour of Said and Yarg Salem, two brothers born into slavery, and whose former masters were prosecuted but given very lenient sentences.
MRG has also focused on training minority youth activists, often giving them the encouragement and confidence to realize their dreams of devoting their lives to human rights work. Zola Kondur, a Roma activist from Ukraine, talks about how a training programme she worked on with MRG supported young community members to go and speak at international meetings: ‘This was first time they spoke at this level. They were stressed and nervous but they did it really well, and they did networking.’ One such activist went on to be appointed by a local authority as adviser on minority issues, with a budget to implement activities – a ‘unique case in the Ukraine’, according to Zola.
Photo: A human rights training session in Gumare, Botswana
-
By Chris Chapman
Salimata Lam has been an activist all of her adult life, since joining a pro-democracy movement in her teens. In the 1980s, she was even deported from the country for three years and stripped of her citizenship, which only made her more determined to be an activist. ‘I saw that the system was unjust. It strengthened my resolve to combat injustice.’ She has been advocating with the Mauritanian NGO SOS Esclaves against modern forms of slavery since 2010.
As a long-term partner of MRG, Salimata points to how SOS Esclaves has benefited from the cooperative relationship. ‘The dialogue with the state is difficult. Their position is that slavery does not exist. MRG and other partners help us to collaborate with intermediaries, who communicate our recommendations.’ An example of this is the work at the African Commission on Human and Peoples’ Rights, including the child rights committee, whose ruling has been instrumental in pressuring the government to live up to its commitment to end slavery.
Her organization has worked together with MRG to train activists, journalists, paralegals and magistrates. As a result, not only have she and her staff been able to learn through the experience of implementing large projects, they have also benefited from being exposed to the content of training programmes. ‘I have really benefited from the workshops on how to use the media,’ she says:
‘Public opinion is very important. What we need is to work on deconstructing the existing mentality. If slavery persists, it’s because that work of deconstruction is not yet finished, so that people will say no.’
Salimata sees progress, even if it is slow: ‘Fifty years ago, if you called someone a Haratine, they would be insulted. Today, the people say, yes we are Haratine. They are ready to assume their identity. People want to be free, to live in dignity. This tendency is irreversible.’
Photo: A portrait of Salimata Lam
-
By Rasha Al Saba
From conflict to climate change, MRG has repeatedly reoriented its work in the face of new crises to ensure that minorities and indigenous peoples – frequently the most affected by these challenges – are not forgotten. Most recently, in the wake of the outbreak of Covid-19 at the end of 2019, we have focused much of our efforts on understanding the implications for the most marginalized populations across the world. From the early stages of the pandemic, it was clear to us that minorities and indigenous peoples would likely be disproportionately affected.
Today there are millions of cases of Covid-19 globally, with thousands of new cases being confirmed every day. The Covid-19 pandemic is, at root, a public health emergency, driven by its ready transmission and ability to cause severe illness and death. But while its ability to overwhelm the best of health systems has already been demonstrated, its farreaching social, economic and political consequences are still unfolding with minorities and indigenous peoples among the worst affected.

Ethiopian domestic workers wearing masks sit together with their belongings in front of the Ethiopian consulate in Hazmiyeh, Lebanon / Reuters/Mohamed Azakir. Mounting evidence shows that minorities are at greater risk of contracting the virus for a range of reasons – disproportionate employment in high-risk sectors, concentration in overcrowded housing, and higher mortality rates post infection often due to poorer health status and limited access to medical care. While less data was initially available concerning the impact of the pandemic on indigenous communities, emerging evidence suggests that the implications have been ‘disproportionately devastating’.
The disproportionate impact of the virus has also extended to minority and indigenous communities’ livelihoods and security, access to basic services, education and food with women and people with disabilities within communities further exposed to negative impacts. Fears grow of the implications of the pandemic for minorities and indigenous peoples in the global south, largely undocumented due to a lack of data or reporting.
Covid-19 developed into a crisis of human rights as well as public health, exposing deep inequalities and the fragility of global health and protection systems. Minorities and indigenous peoples face an even more hostile environment, characterized by increasing racism, xenophobia and scapegoating. In addition, the wide ranging containment measures by governments had profoundly discriminatory impacts on the most marginalized in societies visible in the mistreatment, detention and deportation of migrants, refugees and asylum seekers in the name of containing the virus.
While lockdown measures aimed to slow viral transmission, their unintended consequences have been far reaching, devastating livelihoods, disrupting schools and closing borders. These impacts, distributed unevenly, brought renewed urgency to the situation of minorities and indigenous peoples worldwide, with many concerned that the pandemic could reverse modest advances in improving social and economic equality.
It is clear that the pandemic has aggravated pre-existing social and economic inequalities for marginalized communities, including minorities and indigenous peoples. With risks of recurrent outbreaks high, it is crucial to support and protect the most vulnerable to effectively control the virus. Efforts to examine the disproportionate impact of the virus on racial and ethnic minorities must be scaled up and adopted widely to include religious, linguistic and other aspects of social identity. To understand what is behind the greater vulnerability of some groups to Covid-19, policy makers and scientists must focus more attention on the social determinants of health and explore how these intersect with ethnicity, race, religion, language and disability. Lessons from this pandemic should be learned, and opportunities for possible synergies with human rights and development agendas must be taken. To reverse inequalities and discrimination brought on by the pandemic, it is important to prioritize measures to guarantee social and economic rights, while delivering on the commitment of ‘leave no one behind’. In immediate terms, this should include issues relating directly to the pandemic. For example, governments should ensure that vaccines, when developed, will be delivered on the basis of vulnerability to exposure, including due to socio-economic or health roles, rather than on the ability to pay or membership of a dominant ethnic, religious or linguistic group.
However, the broader synergies between the immediate crisis response lie with the longer-term realization of the Sustainable Development Goals (SDGs), especially those associated with health, hunger poverty and adequate shelter. Efforts should be intensified to guarantee the right to health and the achievement of SDG 3, including the targets of universal health coverage for all countries, while addressing the national and local barriers that minorities and indigenous peoples, as well as refugees, migrants and people with disabilities, experience when accessing health care. Ultimately, the most fundamental step to address the current crisis and strengthen resilience for future public health challenges is to push for a more inclusive and equitable development landscape for all.
Within days of the announcement of the pandemic in March 2020, MRG reached out to our donors to ask whether we could shift our work to ensure that it remained relevant during the pandemic. Most donors agreed very swiftly and many also agreed that we could include direct aid to affected minority and indigenous communities. This allowed us to reach out to our partner organizations to identify the key supplies that their communities needed. We were then able to support them in providing for excluded communities with a range of Covid-19 related facilities and supplies, from handwashing stations and personal protective equipment to mattresses in remote quarantine centres, as well as cleaning and disinfectant products. We also enabled public health broadcasts on community radio stations in local languages, translation of health guidelines on leaflets and the recording of songs in local languages containing key messages. In a few instances where we had evidence that food distribution was skipping or discriminating against minority settlements and communities, we even provided some food aid or cash for food support for extremely vulnerable households.
To date, MRG has also undertaken a range of research on the social, economic and health impacts of Covid19 on minority and indigenous populations. This includes an extended briefing that examines the different facets of the minority and indigenous experience of the pandemic, such as the factors that render some communities more vulnerable to the spread of the virus, and the particular dynamics of its dissemination in conflict and fragile settings. It also examines the need for better data disaggregation to highlight inequalities, the impact of restrictions on livelihoods and incomes as well as the implementation of discriminatory containment measures for minorities, indigenous peoples and other groups including migrants and refugees.
Building on this, we are currently working with partner organizations in Africa, Asia, Europe and the Middle East, to undertake field studies on the specific impacts of the pandemic on these communities. We have recently begun a collaboration with the Special Rapporteur on contemporary forms of slavery to explore how the vulnerability of minorities and indigenous peoples to exploitation is increasing. We will also focus our 2021 Minority and Indigenous Trends report on Covid-19. Our hope is that, by combining extensive research and advocacy with local community-led programmes, we can help ensure that these groups do not become invisible victims of the pandemic.
—
More information on MRG’s research on Covid-19 is available in the briefing Inequality and the impact of Covid-19: How discrimination is shaping the experiences of minorities and indigenous peoples during the pandemic.
Top photo: A Yanomami child holds a face mask in Brazil / Adriano Machado/Reuters
-
By Neil Clarke
Numbering at least 10 million, though the actual numbers are likely higher, Roma make up the largest ethnic minority in Europe. Roma populations can be found in every country and, while it would be wrong to perpetuate the image that all Roma live in low-income communities, the levels of discrimination, segregation and poverty they have faced throughout their long history in the region is unique. The fact that, regardless of the country they live in, this exclusion continues to shape the experience of Roma to this day highlights the enduring scar of anti-gypsyism in Europe.
However, the 1970s saw real progress in the development of pan-Roma identity and leadership, with Roma leaders and CSOs around the world coming together to demand greater justice and equality for Roma peoples. MRG was a natural ally in the fight to secure Roma rights. In the 1980s, following a spike in attacks on Gypsy, Roma and Traveller communities in the UK, MRG was engaged in developing a number of educational materials that were distributed throughout schools to counter myths and discrimination.
However, over time and with Roma-led civil society growing, MRG’s role became much more about supporting Roma organizations to engage directly with international institutions themselves. In 1995 MRG published the report Roma/Gypsies, written by Jean Pierre Liegeois and Nicolae Gheorghe, a leading Roma activist, and employed a staff member to provide mentoring support for Roma leaders. Subsequently, until 2010, MRG implemented a number of programmes focusing specifically on Roma advocacy in the European Union (EU), first in Central Europe (due in part to the establishment of MRG Europe in Hungary in 1996) and more recently in South East Europe. These programmes used the leverage of the EU accession process, which required new and prospective EU members to ensure substantive safeguards to ensure the integration and protection of national minorities. These changes brought new funding programmes for Roma integration and legal reforms to provide more effective protection against discrimination.
Over time, a number of Roma networks and NGOs were established and have led the way in advocating for Roma rights in the EU, in particular those countries that are part of the Decade of Roma Inclusion. At the same time, as MRG’s work moved into Eastern Europe, we continued to engage in new initiatives with Roma partners across the region, notably in Georgia, Moldova, Russia, Turkey and Ukraine. Throughout these actions, it has become undeniably clear that the proliferation of programmes and funding for Roma integration, often driven by the EU and focusing predominantly on economic and social integration, are continuously undermined by the pervasive, deep-seated nature of anti-gypsyism.
The recent programme in Ukraine, implemented by MRG and the Roma Women’s Fund Chiricli, sought to build new partnerships between local authorities and Roma CSOs through many successful and innovative integration programmes. Yet, at every stage many of these achievements occur against a backdrop of continuous racism. It is undeniable that, without recognizing and addressing the phenomena of anti-gypsyism, equality and inclusion for Roma will never be fully attained.
In this context, recognizing the impact of the internet in spreading and disseminating hate speech, MRG began our first intervention in combating online hate in 2017 with the Freedom from Hate (FFH) programme. While many cyberhate initiatives focus on monitoring and prosecuting hate speech, this programme focused on developing counter-speech strategies online. This was in response to the fact that the internet is now the primary forum for public debate and that, while standards for minority rights may exist in conventional media such as newspapers and television, social media is developed in private spheres outside these norms. Access to public debate on the internet is now a crucial challenge in ensuring the social inclusion of minorities and freedom of expression, particularly as social media allows people to operate in often closed information silos.
The FFH programme deliberately sought to develop cooperation between both Roma and non-Roma CSOs, as it has often been the case that anti-racism initiatives in Europe have themselves excluded Roma. One of the key results of this collaboration was in formulating strategies that identified and challenged the link between stereotyping and how this evolves into more explicit forms of hate. In this way, the programme began to address the structural nature of online anti-gypsyism. Alongside the FFH programme, MRG has also developed a new body of programmes, following pilot initiatives in Macedonia, that utilize new technologies to create a network of virtual legal advice services for Roma in Central and South East Europe.
As an ally to the Roma rights movement, MRG’s work with our Roma partners now forms the largest and most varied component of our work in Europe. But it is important to remember that discrimination against Roma is not only a European phenomenon. MRG has been supporting activists protecting the rights of Roma in Iraq for a number of years and is developing new initiatives for Central Asia and Middle East and North Africa (MENA) regions. In the years ahead, it is critical that MRG and other allies of the Roma rights movement, continue to focus on interventions that address the systematic and structural causes of anti-gypsyism, including cyberhate and, particularly in Europe, work to ensure that the broader retrenchment of liberal democratic norms does not expose the Roma to even greater risk of marginalization and persecution.
Photo: Two boys from the Roma community in Zakarpattia, Ukraine
-
By Sofia Olins
When I first met Rosa Iris, she was completing her law degree while raising her 6-year-old son alone. This, in the compromised conditions of a bateye (a town of corrugated shacks with no water and electricity), is no easy task.
Surrounded by sugar cane, we waited for her to arrive so we could film the workers in the fields. She greeted us with warmth and kindness. Straight away I knew she would be a great person to feature in our film Our Lives In Transit.
Jump forward a few months and we had begun shooting our film, Our Lives In Transit. Our previous documentary, about MRG’s first and ground-breaking street theatre project in the Dominican Republic (DR), focused on the programme as a whole. This time, however, we wanted to have a person at the centre of this story – and I knew, almost from the moment we were introduced, that that person should be Rosa. A film about her fight for the rights of her community and all others who were suffering the same discrimination.
MRG has a long history working with Dominicans of Haitian descent in the DR, whose lives continue to be shaped by racism to this day. Numbering up to a million people, many of whom have been resident in the country for generations, they are still confronted by shocking levels of inequality. This includes hundreds of thousands of community members with valid claims to citizenship who are effectively stateless.
But to truly capture the reality she and others faced, we had to film with Rosa over longer periods. We found a way to do this over the course of a year with a local crew while I directed from London via Skype, and with detailed story boards. With MRG’s enthusiastic support, we were able to successfully complete the film under these unusual conditions.
Rosa had told me about how, before her Haitian father had died, she had got to know him better in his later years. We therefore decided that the film could be narrated by her, in the form of a letter, to her father. Over the year, the seasons would mark her mission: to challenge the government’s discriminatory policies and, in doing so, defend his name.
This narrative gave us, the audience, the opportunity to connect personally with Rosa, and through her with thousands of others facing the same plight. The benefit of this approach – film making driven directly by the thoughts and actions of the participants – is that their story can be told with an urgency that delivers greater empathy and understanding to encourage change, which is the ultimate aim of all the documentaries MRG has helped produce.
Our Lives in Transit was screened for UN policy-makers in Europe and at other events in Barcelona, London, Madrid and Asturias, as well as at a high-profile advocacy event in Washington, DC. It also had a further 19 extra screenings at film festivals and events in Canada, the United States, Puerto Rico, Chile and South Africa, not to mention in DR itself, attracting tens of thousands of viewers in the process. This, and an extended advocacy campaign around the film, led to great visibility around the issue of statelessness in the DR and other countries. Not only were governments engaged and challenged, but a rarely told story affecting hundreds of thousands of people was shared with the wider world – an important step towards improved understanding.
Photo: Dominican Republic Street Theatre programme
-
By Miriam Puttick
In conflict zones around the world, violations against minorities are often an inseparable element of the core conflict dynamics. States and armed groups will often harness long-standing tensions and stoke hatred against minorities as they vie for power and resources, while the escalation of conflict can exacerbate the vulnerability of already-marginalized groups.
In Iraq, for example, the rise of the so-called Islamic State of Iraq and al-Sham (ISIS) and other armed groups from 2014 onwards saw patterns of marginalization of the country’s ethnic and religious minorities transform into widespread attacks and even genocide against those communities. Ethnic and religious minorities were uprooted en masse from their historical homelands and subjected to violations, including killings, abductions, property destruction, and attacks on their religious and cultural heritage. Footage of these atrocities was disseminated widely across social media platforms, which ISIS used with shocking efficiency to spread its ideology and recruit new members.
Monitoring violations of human rights and international humanitarian law in conflict zones often poses immense challenges. For one thing, the existence of armed violence often prevents human rights organizations, journalists, UN agencies and others engaged in monitoring from accessing the territories where violations are occurring. Local human rights actors, for their part, may become displaced or preoccupied with their own survival needs. When they do choose to continue their work, they operate at increased risk to themselves, often facing death threats from armed groups for speaking out or exposing violations. In situations where minorities are disconnected from centres of influence or lack organizations defending their rights, violations can go completely unreported. Moreover, the high degree of political polarization that accompanies conflict and attempts by various actors to control the narrative of events often lead to difficulty in gathering accurate and impartial information on the human rights situation.
However, this does not mean that there is no information being produced in such settings. Thanks to the spread of mobile internet, social media platforms and smartphone technologies, ordinary civilians are able to document developments on the ground and share them with the outside world at the click of a button — even in the world’s most dangerous conflict zones. Facebook, YouTube and other social media platforms are often awash with first-hand information, photos and videos coming directly from witnesses to violations. The content of social media is becoming difficult to ignore, as seen in the rise of opensource intelligence (OSINT) approaches. However, this content is often not in a format that can be harnessed effectively for human rights advocacy. Information shared online can be difficult to verify and often lacks crucial details needed to establish the nature of the violation and hold perpetrators to account. Moreover, intersecting privacy rules on a multitude of platforms mean that vast amounts of data are often not easily accessible to relevant human rights actors, such as international bodies.
These challenges provided the impetus behind the creation of the Ceasefire online reporting tool, a digital platform that seeks to enable ‘civilian-led monitoring’ of violations of human rights and international humanitarian law in conflict settings.
Piloted in Iraq as part of a joint project by MRG and the Ceasefire Centre for Civilian Rights, the tool seeks to bridge the gap between traditional human rights data collection and unbounded crowdsourcing. Though accessible to anyone with an internet connection, the tool prompts users to report violations in a way that conforms with international legal standards and increases the future usability of the data.
The core component of the tool is a bilingual (Arabic-English) reporting form, which permits users at a minimum to specify the title, description, category and location of the human rights violation. The category function, which prompts users to choose from a predefined list of internationally recognized human rights violations, enables easy analysis and filtering of the data. In addition, the expanded version of the form asks for additional details about the victim, witness, consequences, motive and perpetrator of the violence, prompting users to supply information that could be important in determining the nature of the abuse according to international standards. For example, users are asked to give any details that would suggest the attack was carried out due to the victim’s ethnicity, religion or culture – which can be used to establish the threshold for hate crimes, ethnic cleansing or genocide. Users can also attach photos and other documentary evidence to their reports or include links to YouTube footage or media coverage, which helps make the information verifiable.
Reports submitted through the form are stripped of personally identifying information and plotted onto a live, interactive map visible on the tool’s landing page, which shows the distribution of violations by location and type. Sensitive data, such as names and contact details of victims, witnesses and perpetrators, is stored securely on a secondary server in case it is needed for future follow-up or court proceedings. However, civilian-led monitoring is not simply about providing new technological tools – it is also about empowering civilians themselves so they can use such tools effectively. Through partnerships with human rights NGOs, including minority-led organizations, MRG and Ceasefire conduct regular in-country training events for civilian activists. At the training sessions, participants are not only taught how to use the online tool, but also given a thorough grounding in international human rights concepts and components of strong human rights reporting, including interview techniques, victim protection practices and verification strategies. Also known as ‘bounded crowdsourcing’, the logic of training smaller groups, who in turn train others, leads to the formation of a critical mass of skilled activists and organizations and results in a higher quality of human rights documentation.
Since the tool’s launch in February 2017, more than 3,700 violation reports have been submitted by civilian activists. The online tool has thus served as a window into patterns of violations taking place as part of the conflict in Iraq that would otherwise go unreported. For example, through long-term partnerships and trainings with women’s rights activists in Iraq, the tool has enabled the production of detailed information on the relationship between armed conflict and family-based violence, an under-studied and underdocumented phenomenon. These cases led to the publication of a series of three reports on the topic, and the design of new interventions providing direct support to refugee and displaced women facing gender-based violence.
In situations of escalating violence, the online tool offers the possibility of obtaining crucial information from the ground in real time. When large-scale protests erupted in Iraq in late 2018, reports of excessive use of force by security forces against peaceful protesters began to appear on the online tool. These cases were incorporated into a wider report on repression of civilian activists in Iraq, which was then used as a basis for urgent appeals and advocacy pushes at the UN Human Rights Council and in other forums.
According to the director of an Iraqi NGO, the value of the online tool lies in its ability to function as a secure outlet for activists engaged in human rights documentation in highly volatile contexts. ‘In the current situation in Iraq, the major risk facing human rights activists and defenders is reporting violations. Many activists have faced threats and blackmailing for their reports, particularly if their identity is revealed. The online tool helps them prevent these risks as they easily use the tool and it is anonymous.’
Building on its initial successes in Iraq, the tool has since been expanded to other contexts in the region. Following the Turkish invasion of Afrin in north-western Syria and the mass expulsion of the city’s mainly Kurdish population, the tool served as a crucial platform to document the violations taking place against the population of the area in the midst of a neartotal media blackout. According to a Syrian Kurdish activist from Afrin, ‘Up to now, all independent journalists are barred from entering Afrin, so there are no media or human rights reports covering the situation there. With the Ceasefire tool, we were able to design forms specific to the area and give people on the ground the option of reporting violations over the internet. As a result, we are monitoring the situation without exposing researchers to the dangers of entering the territory.’ Civilian activists were also able to uncover patterns of attack by Turkish-backed Syrian armed groups against Yezidi, Christian and Alawite villages around Afrin, about which very little is known internationally.
While the online tool has provided a way to surmount some of the obstacles to human rights monitoring in conflict, the work has not been without its challenges. Despite all reassurances of confidentiality, victims can still be afraid to report violations — fearing backlash from their families, their communities or armed groups. Where the authorities deliberately shut down or throttle internet access, there can be delays in urgent reports being uploaded online. Moreover, in situations of prolonged violence, even the most committed activists can begin to lose hope that an end is in sight — decreasing their motivation to go on with the documentation work. These challenges prove that technology alone is not enough to resolve the enduring problems of human rights. Sustainable change is unlikely to be achieved unless technology is deployed in conjunction with other measures — from political pressure to legal advocacy and education. However, harnessing technology as part of a multi-pronged approach can offer a modern strategy for dealing with modern challenges, which continue to change the landscape of human rights activism.
Photo: Yezidi refugees who fled ISIL attacks in Iraq / Caroline Gluck-EU-ECHO
-
By Chris Chapman
Mikhael Benjamin is an Assyrian-Christian activist from Iraq who has devoted his life to fighting for the rights of his community, first in a political party, and since 2005 in the human rights movement. Since the beginning of the second Gulf War in Iraq in 2003, religious and ethnic minorities, including the Christians and the Yezidis, have experienced a humanitarian catastrophe of genocidal proportions. These communities have in many cases been driven from their lands, and Mikhael has focused in his advocacy work on protecting land rights and cultural diversity, in particular language rights.
A turning point in Mikhael’s career of activism, he says, came in 2010. He had already been working with MRG for a number of years, participating in its training programmes, and his organization, the Nineveh Center for Minority Rights, had received funding to implement a project on documenting human rights violations. It was at this time that MRG encouraged him to apply for a fellowship programme for minority activists at the UN. He did so, and was successful. This programme broadened his knowledge of the tools at his disposal for campaigning work. As he says:
I came to know that I have the right to advocate for my rights, not only to go outside to demand and to campaign in the street, but also in the legal way, to use international law, to use whatever means and tools, and to use the United Nations system.
Mikhael began to put this holistic approach into practice when he started working on a land dispute in Duhok province, in the Nahla Valley in Iraqi Kurdistan, in 2013, using it as a pilot project. The Nineveh Center for Minority Rights, together with the Assyrian Democratic Movement (the political party he used to be a member of), had been documenting cases of land grabbing by other communities in Assyrian-Christian areas since the early 1990s.
In 2014, they organized a demonstration in front of the parliament of Iraqi Kurdistan to protest against one such case. However, when Mikhael was travelling from the Nahla Valley to Erbil, he found that the police had set up roadblocks and were checking identity cards. In Iraq, these cards identify the religion of the bearer. In this way, the police were able to turn back all Christians travelling to demonstrate. Undeterred, Mikhael engaged with local media and was interviewed about the case on a local TV channel. A week later, the Kurdistan president ordered the destruction of the illegal occupier’s buildings on the land. In order to consolidate this decision, Mikhael lodged a case in the courts, and won in the first instance. However, the land is still occupied, and the current occupants are appealing. In addition, the Nineveh Center submitted information to the UN committee which monitors Iraq’s compliance with the Covenant on Economic Social and Cultural Rights. As a result, this committee recommended that the government ‘put an end to illegal expropriation of Assyrian lands without compensation or the provision of alternative accommodation’ and to ‘ensure that judicial decisions ordering the return of lands to Assyrians are enforced’.
Mikhael’s organization has also successfully lobbied to have a law adopted in Kurdistan for the protection of the rights of ‘components’ – the terminology used to describe minorities – and is working with both Kurdistan and central governments to develop a school curriculum that is inclusive of minorities. But in the end many laws and polices are not implemented, and remain tokenistic gestures. The same, says Mikhael, is true of their representation in parliament.
They tell us that in Kurdistan, we have five seats in parliament, even though we are a very small community. But those five seats are not completely representing our community because political parties put those people there. I learnt this from the fellowship programme: we need real and effective political and economic participation – it should not be décor.
Photo: Women celebrate an Easter Mass at the Syrian Orthodox Mart Shmony Church in Bartella, Iraq / Teun Voeten
-
By Lucy Claridge
In 2017, the African Court on Human and Peoples’ Rights issued its first ever ruling on indigenous rights in a case brought by MRG in partnership with Kenya’s Ogiek community. Numbering around 30,000 people, the Ogiek are some of Africa’s last remaining forest dwellers. Traditionally honey-gatherers, they survive mainly on wild fruits and roots, game hunting and traditional beekeeping. Having inhabited the Mau Forest for many centuries, their unique way of life is closely tied to its rich biodiversity and natural resources: in fact, the term ‘Ogiek’ literally means ‘caretaker of all plants and wild animals’.
Since independence, and indeed prior to it, Ogiek have been routinely subjected to arbitrary forced evictions from their ancestral lands by the Kenyan government, without consultation or compensation. The Ogiek community’s rights over their traditionally owned lands have been systematically denied and ignored, with the Kenyan government allocating land to third parties, including political allies, and even permitting substantial commercial logging to take place. The eviction, without compensation or consent, of Ogiek from their ancestral lands and the refusal to allow them access to their spiritual home has prevented the community from carrying out their traditional practices and their hunter-gatherer way of life. As a result, their very existence is threatened.
In a landmark judgment, issued in May 2017, the Court found that the Ogieks’ rights to property and natural resources, non-discrimination, religion, culture and development had been violated. The Court also made some very clear rulings in relation to the role of indigenous peoples, and specifically hunter-gatherers, in conservation – rulings that are crucial to the fight against climate change. The Court clearly stated that the preservation of the Mau Forest could not justify the lack of recognition of Ogieks’ indigenous or tribal status, nor the denial of the rights associated with that status. It also explicitly confirmed that the Ogiek community could not be held responsible for the depletion of the Mau Forest, nor could it justify their eviction or the denial of access to their land to exercise their right to culture.
These edicts will be of huge relevance to other forest communities that have been evicted from their traditional lands in the name of conservation, including Sengwer in Western Kenya and Batwa from Kahuzi-Biega National Park in Democratic Republic of Congo DRC, a community on whose behalf MRG is also currently litigating. In the words of Daniel Kobei, Executive Director of the Ogieks’ representative organization Ogiek Peoples Development Program:
[T]he Ogiek journey in the corridors of justice, from Kenya to Banjul then Arusha, was never a bed of roses, it had ups and downs, but thanks to MRG’s support throughout, the litigation process was a success. We don’t know how the Ogiek case would have turned out without partners like MRG standing by us – and they are still by our side, supporting in all aspects. We are indeed indebted to them for their teamwork, especially fraternity.
Photo: Ogiek cultural day, April 2017 / OPDP
-
By Lucy Claridge
MRG’s strategic litigation programme was established in 2002, in response to the clear need for specific legal tools to combat violations of the rights of minority and indigenous communities throughout the world. It aims to improve the capacity of minorities and indigenous peoples to access the legal protection afforded by international instruments on human rights and the various bodies that enforce them. The programme holds governments and other private actors to account for human rights abuses, by bringing landmark test cases before regional, international and domestic bodies.
The legal programme also builds the capacity of local minority and indigenous communities and those representing them to both monitor human rights abuses during the course of the litigation and related advocacy, and to demand the implementation of their rights outside the framework of the programme. This includes the provision of paralegal training specifically developed to match the needs of each community, and training on how to advocate for rights before regional and international mechanisms.
Over the years, it has become one of the leading human rights litigation programmes on minority and indigenous issues, covering many thematic areas such as descent-based slavery (in West Africa), political disenfranchisement and discrimination in accessing public services (in Eastern Europe and Southern Africa), and access to and enjoyment of ancestral lands (across East and Central Africa).
Land rights litigation was commenced by MRG on behalf of indigenous communities as an effort to find solutions to historically embedded land disputes. While much of the world’s land is held communally by indigenous peoples and other communities, under systems of traditional and collective ownership, many governments fail to recognize these claims. As a result, their territories have frequently been allocated to investors for other uses, including development, agribusiness, tourism and conservation. For indigenous peoples, which have deep spiritual, cultural, social and economic connections with their lands, making them central to their identity and indeed their very existence, the effects are catastrophic.
As the effects of climate change intensify and the pressure to take steps to address its consequences mounts exponentially, there has been increasing recognition that indigenous peoples – hunters, fishers and herders – have a central role to play as environmental stewards. In fact, although indigenous peoples make up less than 5 per cent of the world’s population, they are believed to safeguard as much as 80 per cent of the world’s remaining biodiversity. Dependent on their communally owned lands for their survival, indigenous peoples possess in-depth, traditional knowledge of how best to conserve natural resources, protect biodiversity, and mitigate or adapt to the effects of climate change.
Yet governments and other key international actors have done little to cultivate indigenous peoples as allies, preferring instead to adopt the ‘fortress conservation’ model – an approach that often involves the eviction of indigenous inhabitants from forests and other areas in the name of environmental protection. This is despite research showing that this not only results in serious human rights violations but is also ineffective in achieving its aim as it side-lines the traditional knowledge and lived experiences of communities – vital assets in ensuring the sustainable use and preservation of natural resources and ecosystems.
One particularly egregious example of this is the displacement of Kenya’s indigenous Endorois from their ancestral lands in the 1970s to create the Lake Bogoria National Reserve, now a UNESCO World Heritage Site. In 2010, MRG secured a successful ruling from the African Commission on Human and Peoples’ Rights in favour of the Endorois, declaring their eviction illegal and finding that the Kenyan government had violated certain fundamental rights of the community protected under the African Charter on Human and Peoples’ Rights and other international instruments. Building on this success, MRG has supported a successful claim by the Ogiek community to return to their land in Kenya’s Mau Forest.
Photo: An Ogiek woman on her ancestral lands, Mau Forest, Kenya
-
By Chris Chapman
From the outset in 1970, MRG reported on many areas of violent conflict where the rights of minorities and indigenous peoples were denied and where others remained silent for fear of being associated with secessionists or ‘terrorists’. By 1990, the wide range of contexts and communities covered by MRG included Northern Ireland, Eritrea and Tigray, the situation of Basques and Catalans in Spain, Nagas in India, Kurds, and Palestinians, as well as other areas such as Burundi, Cyprus, East Timor, Lebanon, Uganda and Sudan.
More were to follow. In 1990 MRG became heavily involved in the CSCE/OSCE processes following the ending of the Cold War. A violent conflict was already underway between Armenia and Azerbaijan, there were ominous signs of an imminent violent conflict in Yugoslavia, and major tensions were developing elsewhere.
MRG had a two-pronged approach. Firstly, it worked for the establishment of the OSCE’s High Commissioner on National Minorities with a strong conflict prevention mandate and in due course supported their work. Secondly, MRG worked closely with the Helsinki Committees and minority communities throughout Europe to promote the realization of minority rights, ultimately leading to the creation of MRG’s regional office in Budapest in 1996.
MRG’s work on preventing, managing and transforming conflicts focused on identifying the causal links between violations of the rights of minorities and indigenous peoples, and the onset of violence. The organization also advocated with decision-makers – both at the national level and in international organizations such as the UN – to have those causal links understood and addressed in policy and practice. Furthermore, it provided practical support to communities living in, or emerging from, conflict situations through research, capacity-building and advocacy support.
Before the organization embarked on this work, various studies had already found that many conflicts would be avoided if ways were found to incorporate minorities into public life and respect their rights. MRG set out to understand better how specific aspects of minority rights violations – such as hate speech and hate crimes, denial of identity, and exclusion from political processes, economic livelihoods and state services – were linked to the outbreak of conflict. In a qualitative study of conflicts between 2007 and 2013, the organization found that 71 per cent of the world’s conflicts were linked to tensions involving minorities and indigenous peoples.
This is not to say that minority and indigenous communities have themselves been active participants in the violence: in most cases, in fact, these groups have primarily been targeted by armed actors, such as state or paramilitary groups. In the Democratic Republic of the Congo (DRC), for example, MRG provided evidence to the International Criminal Court that the warlord Jean-Pierre Bemba persecuted and tried to exterminate the indigenous Bambuti people in Ituri province as part of a drive to control territory and access precious minerals, in a conflict in which Bambuti were themselves innocent bystanders. Similarly, in Rwanda, during the genocide in 1994, the state unleashed deadly violence on the Tutsi community, and indigenous Twa were often caught in the crossfire.
Even in cases where communities have themselves taken up arms, this has generally occurred against a backdrop of protracted discrimination and exclusion. In Nicaragua, for instance, MRG’s research showed how, for some 200 years, the indigenous and Afro-descendant communities of the Atlantic Coast were cut off from economic development, while their unique cultures and languages were denied by a central government wishing to create a homogeneous European-oriented national identity. It was only in the 1980s, following the imposition of a Spanish-language literacy programme on the Atlantic Coast, that community members took up arms against the government.
It is of course one thing to identify the problem, and another to find solutions. MRG lobbied governments and intergovernmental organizations such as the UN to include a minority rights lens in their work to prevent and manage conflicts. Surprisingly, however, a study by a UN expert, for which MRG provided research support, found that agencies tasked with conflict prevention and resolution had no access to expertise on minority rights and did not include a minority rights lens in their policies and approaches.
In Cyprus, Iraq, Egypt, Nicaragua, Fiji, Sri Lanka and other countries, MRG supported local communities in pressuring governments to include them in peace-building efforts. In East Africa, MRG prioritized small-scale, grassroots interventions to tackle local-level conflicts over land, which could escalate and lead to many deaths and loss of livelihoods for remote communities already experiencing deprivation. For example, in Kenya’s Rift Valley, the organization supported a local community NGO, Samburu Women for Education and Environment Development Organization, to strengthen communications between Samburu and Pokot elders, helping to diffuse tensions over livestock and land. The NGO also worked to ensure women’s participation in the traditionally male elders council.
Photo: A Tamil child displaced by civil war living in the damaged remains of a railway station in Sri Lanka / Howard Davies
-
By MRG’s former Head of Programmes
In my time at MRG, we worked on numerous programmes on Freedom of Religion or Belief (FoRB). We advocated for an end to the death penalty for apostasy in Mauritania. In India and Bangladesh, we challenged discriminatory narratives in textbooks and in Indonesia we helped produce animated comics to promote religious tolerance. In Pakistan, Egypt, Tunisia, Iraq, Iran and Sri Lanka, we shone a light on discrimination against religious minorities including Bahá’i, Christians, Muslims, Hindus, Sabean-Mandaeans, Jews, Ahmadis, Quranists, and Yarsanis.
FoRB programmes are tricky to design and implement. They touch on issues that are sensitive for reasons unique to each context, and it is not easy to define goals that are sustainable, safe and achievable in the lifespan of a programme.
The most challenging FoRB programmes are ones that touch on laws concerning blasphemy. Blasphemy has been defined by USCIRF (US Commission on International Religious Freedom) as ‘the act of expressing contempt or a lack of reverence for God or sacred things’. Sixty-nine countries prohibit it in their constitutions, civil codes or penal codes, seeking to punish individuals for allegedly offending, insulting or denigrating religious doctrines, deities or symbols, or for insulting religious feelings. Such laws are enforced to different extents by different states, with penalties varying from death to imprisonment and fines. In some countries, these laws exist in a de facto manner (not explicitly mentioning blasphemy but functioning to that effect) and in yet others as ‘dead letter laws’ (they are on the statute books but no longer enforced).
The human rights community is unified in agreement about the non-compatibility of blasphemy laws with other fundamental human rights. But an interesting disagreement exists on the best advocacy approach. There are broadly two positions. One is the idealist position, which says: ‘We must advocate for the repeal of blasphemy laws because by asking for anything less, we would effectively be agreeing to the violation of other rights.’ The other is the pragmatist position which says: ‘One step at a time – let’s first advocate for the laws to be reformed, rendering them less dangerous and discriminatory. We’ll get to repeal after that.’ I have seen both these positions in action.
In 2012, I met human rights activists and politicians in Pakistan, not long after the assassinations of two prominent politicians, Salman Taseer and Shahbaz Bhatti, for their opposition to Pakistan’s blasphemy laws. The atmosphere of fear in the aftermath of these killings was palpable and it appeared to have given rise to a culture of silence about human rights violations, particularly in relation to blasphemy laws. Though most activists considered blasphemy laws to be anti-human rights, they had tempered their advocacy asks to fit the socio-political climate. They were not asking for these laws to be abolished. Their goal was more modest: to ensure that the laws were not used to victimize innocent people. As things stood, blasphemy accusations were often maliciously used to settle personal vendettas, criminal charges were filed based on abysmally low evidentiary thresholds, and blasphemy accusations all too often catalysed deadly vigilante action with impunity for perpetrators. Members of religious minorities in Pakistan told me that the merest suggestion of blasphemy was in effect a death sentence for the ‘accused’. The rule of law just didn’t apply in any meaningful sense.
The best way to get urgent improvement and protection for those being victimized by blasphemy laws, many activists said, was swift legal reform; repeal could come later. Their reform wish list included making laws less vague, having legally qualified persons vet allegations and evidence before accusations turned into criminal cases, making the formulation and application of laws free from political or other interests, protecting accused persons from vigilante action, and making penalties proportionate. In short, this was a pragmatist advocacy stance.
I discussed this position with the then UN Special Rapporteur on freedom of religion or belief, Dr Heiner Bielefeldt. His position was that such laws do or could contravene, in intent or in practice, international human rights norms and obligations, including the right to privacy, the right to life, the right to physical and mental integrity and the right to freedom of expression. They tend to privilege the protection of one or some religions or beliefs over others and often deviate from principles of proportionality of punishment and non-discrimination and equality, and the principle of legality which requires precise and unambiguous language to define a punishable offence. While understanding the pragmatist position, Mr Bielefeldt felt that even if the ideal outcome was unattainable in the near term, we must not water down our advocacy asks. We must always and unequivocally demand rights in their fullest form. In this context, that could only mean the abolition of blasphemy laws.
It is no surprise that national actors are often pragmatic, and international actors idealist. The latter have a mandate to promote and secure human rights, and for them it is impossible to advocate for anything less than the internationally agreed human rights standards; to do so risks being seen to agree that the full standard in not applicable in any given context, which is never the case. Local actors, on the other hand, know that advocating for the full standard may mean that no progress is made; given the horrifying impacts of blasphemy law cases, any progress is seen as better than nothing.
Ultimately, the idealist and pragmatist positions are not contradictory. Both eventually pull in the same direction and towards the same goal, albeit with varying conceptions of how to get there and how long the journey should take. MRG’s role is to provide a bridge so that national and international actors can work together and collaborate in safety, making maximum efforts to achieve the change that religious minorities around the world so clearly need. Every effort, idealist or pragmatist, to question and challenge blasphemy laws contributes to holding governments and the international community to account for their human rights obligations.
Photo: A Sikh devotee waits to take part in a religious ceremony during the Baisakhi festival at Panja Sahib shrine in Hassan Abdal, Pakistan / Saiyna Bashir/Reuters
-
By Silvia Quattrini
Freedom of Religion or Belief (FoRB) is usually defined as the freedom to adopt, change or renounce a religion or belief and it involves principles such as freedom of worship and freedom from coercion. Unnecessary restrictions to FoRB of religious minorities, such as restrictions on places of worship, but also restrictions that might limit access to other basic human rights, such as lack of official recognition and registration requirements, are still widespread all over the world.
According to Claire Thomas, Deputy Director at MRG:
For decades, FoRB human rights work largely centred on advancing freedom of worship, and not freedom from persecution and discrimination because of one’s religious identity or beliefs – even though both facets are included in the main UN Convention articles. A shift in the international understanding and attention to FoRB occurred with the genocides of the Yezidis in Iraq and the Rohingya in Myanmar.
Historically, MRG has been one of the few non-faith-based organizations working on FoRB and on the rights of religious minorities more broadly. Our first ever report, originally published in 1970, was on this very topic: Religious Minorities in the Soviet Union. Since then, we have produced dozens of publications examining the situation of religious minorities in different parts of the world. In particular, MRG has produced a series of reports on Iraq and the challenges faced by religious minorities, including Bahá’is, Christians, Jews, Sabean-Mandaeans, Shabaks and Yezidis, from the US-led occupation in 2003 to the rise of ISIS.

A Sikh devotee waits to take part in a religious ceremony during the Baisakhi festival at Panja Sahib shrine in Hassan Abdal, Pakistan / Saiyna Bashir/Reuters. Since MRG as an organization started moving to a project-based approach in the late 1990s, much of our work on the topic followed this shift. This does not mean that MRG stopped conducting research into FoRB around the world, but rather that a multidimensional approach was put in place, through activities in partnership with local organizations, with topics of research often guided by the findings of these projects. Much of this work focused on the Middle East and North Africa (MENA) and South Asia, as the threats to religious minorities in those regions escalated significantly during this time.
MRG’s first prototype project was launched in 1996 as part of the publication of The Copts in Egypt and followed by the ‘Religious Minorities in Asia’ project, launched in 1999. Several other projects were then implemented, with the aim of protecting and promoting freedom of religion or belief and the rights of religious minorities through capacity-building, creation of networks, media awareness, research and advocacy at both national and international levels. Our programmes have sought to promote stronger ownership by minority organizations themselves, not only through local initiatives such as interfaith dialogues and media engagement, but also at the international level through the participation of dozens of religious minorities activists at key UN events.
MRG has also repeatedly stressed the need for a comprehensive approach that takes into account other human rights standards, such as the right to privacy and freedom of association, as well as principles of equality and non-discrimination, for instance by recommending states to review burdensome registration requirements that have a discriminatory impact on religious minorities. Employing an approach that goes beyond FoRB means that we have been able to work more generally on anti-discrimination, as well as on the economic and social rights of persons discriminated against because of their religion or belief, as it is the case for our current project on Promoting Religious Equality for Inclusive Development in Iraq and Pakistan (2019–22).
At the same time, our work may at times have been circumscribed by the specific objectives and needs of the projects, a challenge of the past 20 years that is not specific to MRG only but reflective of how the NGO world has sustained itself. The limits that this approach brings to the way in which we have been operating have been at the centre of MRG’s internal conversations for the last couple of years. In particular, following worldwide Black Lives Matter protests, we have been questioning not only the existence of structural racism within our own organization and how to better fight against it, but also our positionality as an international organization headquartered in London and the risk of being associated with western interests and agendas, particularly in our work on FoRB in the MENA region. Although a clear-cut solution has not yet been found, this ongoing discussion attests to the flexible and self-critical nature of MRG. While trying to increase our core-funding as a way to rely less on specific project budgets, our ultimate responsibility lies with the marginalized individuals and groups we have been working for and with for the past 50 years, including religious minorities.
Top photo: Coptic children in Minya, Egypt / Luis Dafos/Alamy
-
By Claire Thomas
MRG is not an organization that has set out to be innovative for its own sake: however, it is an organization that listens hard to the people whose interests it exists to serve. And this commitment to listening to the communities we work for does involve being willing to change how things are done – and being willing to do them in ways that are often very different to most other human rights organizations.
An early example of this is our support for minority and indigenous community members to speak at events themselves, not speaking for them. This was essential for MRG because the communities we work with are so often silenced or ignored. Allowing them the space to be heard directly, without the traditional ‘gatekeeping’ role of international NGOs as middlemen, was an essential first step towards ensuring their needs were met in a sustainable way. MRG was already doing this in the early 1980s, at a time when most organizations still had specialist staff who attended advocacy events and the actual voices of survivors of human rights abuses were still rarely heard in Geneva or New York.
Although this is clearly the right approach, it does come with costs and risks: everything from difficulties getting visas to the risk that a spokesperson may say something deeply undiplomatic, putting in doubt MRG’s continued ability to bring people to the same forums in future. MRG worked hard to overcome these potential downsides, proving that it could be done and showing that decision makers reacted very positively to the authenticity, directness and impact that this brought to proceedings. Doing advocacy in this way is now common practice.
MRG’s ability to change has been helped by the fact that it has stayed small. There have never been more than four layers of staff, so only ever two people between the most junior staff member and the director. It has also been blessed with senior managers who tend to avoid hierarchies and who are willing to listen. The fact that MRG has, at times, straddled the divides between the development, anti-racism and human rights sectors has meant that we have been exposed to methods from all three. From Operation Black Vote in the UK, to participatory rural appraisal, to gender mainstreaming and multiple discrimination, MRG has absorbed lessons from imitating others or from recruiting staff who have experience using other methods.

Yezidi men rebuild religious temples that were destroyed by ISIS in Bashiqa, Iraq / Andrea DiCenzo/dpa. From early on, MRG has also committed not only to evaluate all its programmes, but also to make all the evaluations publicly available – a decision that continues to set us apart from most other organizations in the development and human rights sectors. MRG managers communicate to staff (and, importantly, really mean it) that if our work includes no mistakes, nothing that could be done differently and better, then we are not doing a good job. It would mean that we were not taking risks, not trying new things, not listening and not learning. Indeed, donors have themselves responded positively, with feedback suggesting that reading evaluations with honest assessments of what could have been done better is refreshing and reassuring: this ability to critique our own programmes shows that MRG is well run and committed to continuous improvement. MRG staff work hard to ensure that lessons learnt from evaluations in one area are fed into new programme designs, with a series of potentially replicable ‘Learning from evaluation’ points discussed at Council meetings and shared with all staff.
MRG is not at the forefront of every area of innovation, of course. Our small staff and project-based funding make it harder to invest significant time in innovations that have significant upfront costs, such as new technologies and social media. MRG’s size and structure make it more suited to incremental changes that often involve developments out of existing practices, rather than rapid, radical new departures. We are happy to allow other larger, better funded organizations to explore expensive new developments and then learn from their progress.
MRG’s work has also been distinctive in our focus on social and economic rights, such as education and health, at a time when these areas were receiving little attention elsewhere. This still holds true for our work on cultural rights and the use of culture to achieve improved human rights. Again, this stems from the fact that culture is an essential element of what being a member of a minority or indigenous community is all about. It also arose because MRG was aware that social attitudes were falling well behind legal or policy changes – legal reform was important, but without work to transform prejudices on the ground, discrimination would persist regardless.
This is illustrated by the situation of Dalits in India. Although discrimination against Dalits has been illegal for decades, in practice it continues on a daily basis because it is embedded in social attitudes. To challenge discrimination, you need to engage directly with individuals and encourage them to reconsider views they have often been taught since they were children. This insight led MRG to run a series of ground-breaking street theatre programmes that engaged audiences with humorous and thought-provoking plays that also pushed them to rethink their own assumptions, with the majority of audience members retaining the key messages long after.
MRG will continue to listen to the communities it serves, and work in ways that push human rights systems adapt to and meet their needs, and not vice versa.
Top photo: A Dominican woman of Haitian descent
-
By Yulian Kondur
Hate crime has become an increasingly pressing issue in Ukrainian society, particularly since the beginning of 2018, when the number of attacks on representatives of the Roma community and LGBT+ groups has risen. Violence was manifested in a series of pogroms on Roma informal settlements and the murder of a 24-year-old Roma man – as well as the systematic disruption of human rights events and peaceful assemblies or gatherings on gender and LGBT+ topics. While there have been some positive developments in the practice of law enforcement – police have opened investigations into hate crimes against Roma informal settlements, for instance, while Roma NGOs have conducted police trainings and developed algorithms to prevent cases of potential hate-motivated violence – the general climate of impunity persists.
It is also worth noting that many of the positive developments to date on combating hate crime in Ukraine have been driven by continuous advocacy efforts of human rights groups, with Roma NGOs playing an increasingly active role in recent years. The National Roma Integration Strategy has also significantly contributed to the acceptance of Roma NGOs as equal members of the Ukrainian civil society movement. Adopted in 2013 and expiring in 2020, the strategy has been actively utilized by the Roma NGOs to establish cooperation with state authorities and to secure their rights.
In this area, MRG has played a prominent role in supporting capacity-building of Roma NGOs. In cooperation with a local partner, Chiricli, various activities in multiple directions have been organized, ranging from community mobilization and the formation of local advocacy campaigns to pilot projects by Roma NGOs implemented in partnership with local and central authorities. Other actions include holding and participating in national and international advocacy meetings: in particular, in the course of MRG’s involvement in Ukraine, it has focused considerable efforts on advocating for a fairer justice system, including at the UN level.
In the absence of reliable census data, as in Ukraine, studies and mapping can serve as a starting point for collecting information for a needs assessment and gaining a deeper knowledge of the situation of Roma. In this respect, pilot mapping of community needs in several regions has been conducted by Roma CSOs and supported by MRG – so-called ‘Roma social passports’ that have shown great potential and are now being expanded to other regions. This disaggregated data is, among other things, a useful tool for ensuring the security of Roma communities by preventing and combating hate-motivated violence. The Roma social passport itself is a compilation of information collected and processed by local authorities and Roma mediators, reflecting the identified needs and level of access to services among the Roma population in a specific region. It therefore serves to fill the existing knowledge gap in the exact number of Roma residing in Ukraine. The Gender Responsive Evaluation of the National Roma Integration Strategy, conducted in 2019, highlighted the Roma social passport and its methodology as the one of the best practices implemented in Ukraine with regard to improving the situation of Roma.
In its turn, the Coalition of Roma NGOs has continued its involvement in combating hate crimes though monitoring and advocacy. It is currently part of a large-scale project titled ‘United to confront hate-motivated crimes’, coordinated by the Freedom House office in Ukraine and implemented in partnership with the Nash Mir (an LGBT+ NGO), the Congress of National Communities, the Ukrainian Legal Aid Foundation and the Human Rights Centre ZMINA. Among other aims, one of the goals of the project is to bring together the most vulnerable and targeted minority groups in order to assess and map the current challenges, as well as developing viable policy solutions for improving the deteriorating situation in Ukraine in future.
This active contribution by Roma NGOs and civil society is all the more important while the relationship between elements of the state and far-right organizations remains firm in Ukraine – as demonstrated by video footage that emerged of the Minister for Infrastructure, Vladislav Kriklij, accompanying members of the neo-Nazi organization C14 at Kiev Central Railway Station in search of ‘gypsy gangs’. Until these links are severed, the climate for Roma, LGBT+ groups and other marginalized communities in Ukraine will only worsen. Violent ‘anti-gypsyism’ is enabled, first and foremost, by the absence of public sanctions against its perpetrators. This makes the work of Roma NGOs and civil society groups in Ukraine more important than ever.